In 2010, I wrote a series of blog posts on the health properties of potatoes (1, 2, 3). The evidence showed that potatoes are non-toxic, filling per calorie, remarkably nutritious, and can be eaten as almost the sole source of nutrition for extended periods of time (though I'm not recommending this). Traditional South American cultures such as the Quechua and Aymara have eaten potatoes as the major source of calories for generations without any apparent ill effects (3). This is particularly interesting since potatoes are one of the highest glycemic and most insulin-stimulating foods known.
Read more »
Wednesday, December 19, 2012
Friday, December 14, 2012
Thursday, December 13, 2012
Is it Time to Re-write the Textbooks on Insulin and Obesity? Part II
A new paper published on December 6th in the journal Science once again tackles the question of whether elevated insulin drives the development of obesity (1). Mice were generated that lack Jun kinases 1 and 2 specifically in immune cells, impairing their ability to produce inflammation while having very few off-target effects. These mice do not become insulin resistant when placed on a fattening diet, and their insulin levels do not increase one iota. Are they protected from obesity? People who read the last post should know the answer already.
Read more »
Read more »
Labels:
overweight
Monday, December 10, 2012
Does tallness cause heart disease? No, but sex does
Popular beliefs about medical issues are sometimes motivated by a statistical phenomenon known as “spurious relationship”, among other names. Two variables X and Y are influenced by a third variable C, which leads to X and Y being correlated and thus the impression that X and Y are causally associated.
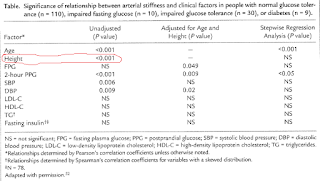
Take a look at the table below, which I blogged about in a previous post (). This table shows that there is a strong unadjusted correlation between height and arterial stiffness, a marker of heart disease. The likelihood that the correlation is due to chance is lower than one tenth of a percentage point (P<.001).
Interestingly, the authors of the study even use height as a control variable to narrow down the “true” causes of arterial stiffness (column with adjusted results), assuming that height did indeed influence arterial stiffness and what they found to be a key predictor of arterial stiffness, 2-hour postprandial glucose.
But there is no convincing evidence that height causes heart disease, with exception of pathological extremes – e.g., acromegaly. Extremes tend to influence statistical results somewhat, leading to conflicting conclusions that end up being disseminated by the popular media (). This is one of the sources of popular beliefs about medical issues.
Another, more important, source are real confounders. And this takes us back to the issue of height being associated with heart disease. In fact, height will typically be significantly associated with heart disease in almost any study that includes men and women and does not control for biological sex.
One of the reasons is that women overall tend to have a significantly lower incident of heart disease than men. The other is that height is significantly lower among women than men, on average, even though there are several women who are taller than the average man.
The table above was from a study including both sexes. Therefore, the strong association between height and arterial stiffness is a “reflection” of the strong association between being male and increased arterial stiffness. If one were to add a variable coded as 0 for male and 1 for female, and use it in a multivariate analysis of predictor of arterial stiffness, together with height, the effect of height would probably “disappear”.
Biological sex is the control variable, the “confounder”, that the authors should have used to narrow down the “true” causes of arterial stiffness (second column in the table). In the absence of biological sex, controlling for height accomplished something similar, but in a “wobbly” way, leaving many readers scratching their heads in confusion.
Take a look at the table below, which I blogged about in a previous post (). This table shows that there is a strong unadjusted correlation between height and arterial stiffness, a marker of heart disease. The likelihood that the correlation is due to chance is lower than one tenth of a percentage point (P<.001).
Interestingly, the authors of the study even use height as a control variable to narrow down the “true” causes of arterial stiffness (column with adjusted results), assuming that height did indeed influence arterial stiffness and what they found to be a key predictor of arterial stiffness, 2-hour postprandial glucose.
But there is no convincing evidence that height causes heart disease, with exception of pathological extremes – e.g., acromegaly. Extremes tend to influence statistical results somewhat, leading to conflicting conclusions that end up being disseminated by the popular media (). This is one of the sources of popular beliefs about medical issues.
Another, more important, source are real confounders. And this takes us back to the issue of height being associated with heart disease. In fact, height will typically be significantly associated with heart disease in almost any study that includes men and women and does not control for biological sex.
One of the reasons is that women overall tend to have a significantly lower incident of heart disease than men. The other is that height is significantly lower among women than men, on average, even though there are several women who are taller than the average man.
The table above was from a study including both sexes. Therefore, the strong association between height and arterial stiffness is a “reflection” of the strong association between being male and increased arterial stiffness. If one were to add a variable coded as 0 for male and 1 for female, and use it in a multivariate analysis of predictor of arterial stiffness, together with height, the effect of height would probably “disappear”.
Biological sex is the control variable, the “confounder”, that the authors should have used to narrow down the “true” causes of arterial stiffness (second column in the table). In the absence of biological sex, controlling for height accomplished something similar, but in a “wobbly” way, leaving many readers scratching their heads in confusion.
Friday, December 7, 2012
Thursday, December 6, 2012
Is it Time to Re-write the Textbooks on Insulin and Obesity?
A recent study in Cell Metabolism by Dr. Arya Mehran and colleagues found a result that, according to a press release, "could overturn widely accepted notions about healthy eating habits" (1), and has set the Internet abuzz.
In this study, researchers generated mice that lack one copy of the pancreatic insulin gene, and compared them to mice carrying both copies (2). Then, they exposed both groups to a fattening diet, and found that mice lacking one copy of the insulin gene secreted less insulin than the comparison group (i.e., they did not develop the same degree of hyperinsulinemia). These mice were also completely resistant to fat gain, while the comparison group became obese. The authors came to some rather large conclusions based on these results, suggesting that the "accepted model" that hyperinsulinemia is the result of obesity is "incompatible with our results that put the insulin hypersecretion genetically upstream of obesity". Ergo, diet causes hyperinsulinemia, which causes fat gain. It's a familiar argument to those who frequent Internet diet-health circles, except in this case the hyperinsulinemia is caused by a high-fat diet.
The problem is that the "accepted model" they want to replace overnight didn't come out of thin air-- it emerged from a large body of research, which was almost completely ignored by the authors. When carefully considered, this evidence suggests an alternative explanation for the results of Dr. Mehran and colleagues.
Read more »
In this study, researchers generated mice that lack one copy of the pancreatic insulin gene, and compared them to mice carrying both copies (2). Then, they exposed both groups to a fattening diet, and found that mice lacking one copy of the insulin gene secreted less insulin than the comparison group (i.e., they did not develop the same degree of hyperinsulinemia). These mice were also completely resistant to fat gain, while the comparison group became obese. The authors came to some rather large conclusions based on these results, suggesting that the "accepted model" that hyperinsulinemia is the result of obesity is "incompatible with our results that put the insulin hypersecretion genetically upstream of obesity". Ergo, diet causes hyperinsulinemia, which causes fat gain. It's a familiar argument to those who frequent Internet diet-health circles, except in this case the hyperinsulinemia is caused by a high-fat diet.
The problem is that the "accepted model" they want to replace overnight didn't come out of thin air-- it emerged from a large body of research, which was almost completely ignored by the authors. When carefully considered, this evidence suggests an alternative explanation for the results of Dr. Mehran and colleagues.
Read more »
Labels:
overweight
Subscribe to:
Posts (Atom)