BackgroundGlucose is the predominant blood sugar and one of the body's two main fuel sources (the other is fatty acids). Glucose, in one form or another, is also the main form of digestible dietary carbohydrate in nearly all human diets. Starch is made of long chains of glucose molecules, which are rapidly liberated and absorbed during digestion. Sucrose, or table sugar, is made of one glucose and one fructose molecule, which are separated before absorption.
Blood glucose is essential for life, but it can also be damaging if there is too much of it. Therefore, the body tries to keep it within a relatively tight range. Normal fasting glucose is roughly between 70 and 90 mg/dL*, but in the same individual it's usually within about 5 mg/dL on any given day. Sustained glucose above 160 mg/dL or so causes damage to multiple organ systems. Some people would put that number closer to 140 mg/dL.
The amount of glucose contained in a potato far exceeds the amount contained in the blood, so if all that glucose were to enter the blood at once, it would lead to a highly damaging blood glucose level. Fortunately, the body has a hormone designed to keep this from happening: insulin. Insulin tells cells to internalize glucose from the blood, and suppresses glucose release by the liver. It's released by the pancreas in response to eating carbohydrate, and protein to a lesser extent. The amount of insulin released is proportional to the amount of carbohydrate ingested, so that glucose entering the blood is cleared before it can accumulate.
Insulin doesn't clear all the glucose as it enters the bloodstream, however. Some of it does accumulate, leading to a spike in blood glucose. This usually doesn't exceed 130 mg/dL in a truly healthy person, and even if it approaches that level it's only briefly. However, diabetics have reduced insulin signaling, and eating a typical meal can cause their glucose to exceed 300 mg/dL due to reduced insulin action and/or insulin secretion. In affluent nations, this is typically due to type II diabetes, which begins as insulin resistance, a condition in which insulin is actually higher than normal but cells fail to respond to it. The next step is the failure of insulin-secreting beta cells, which is what generally precipitates actual diabetes.
The precursor to diabetes is called
glucose intolerance, or pre-diabetes. In someone with glucose intolerance, blood glucose after a typical meal will exceed that of a healthy person, but will not reach the diabetic range (a common definition of diabetes is 200 mg/dL or higher, 2 hours after ingesting 75g of glucose).
Glucose tolerance refers to a person's ability to control blood glucose when challenged with dietary glucose, and can be used in some contexts as a useful predictor of diabetes risk and general metabolic health. Doctors use the oral glucose tolerance test (OGTT), which involves drinking 60-100g glucose and measuring blood glucose after one or two hours, to determine glucose tolerance.
Why do we care about glucose tolerance in non-industrial cultures?One of the problems with modern medical research is that so many people in our culture are metabolically sick that it can be difficult to know if what we consider "normal" is really normal or healthy in the broader sense. Non-industrial cultures allow us to examine what the human metabolism is like in the absence of metabolic disease. I admit this rests on certain assumptions, particularly that these people aren't sick themselves. I don't think all non-industrial cultures are necessarily healthy, but I'm going to stick with those that research has shown have an exceptionally low prevalence of diabetes (by Western standards) and other "diseases of civilization" for the purposes of this post.
Here's the question I really want to answer in this post: do healthy non-industrial cultures with a very high carbohydrate intake have an excellent glucose tolerance, such that their blood glucose doesn't rise to a high level, or are they simply resistant to the damaging effects of high blood glucose?
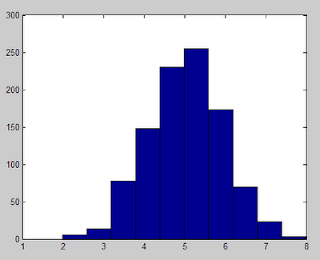
The dataI'm going to start with an extreme example. In the 1960s, when it was fashionable to study non-industrial cultures, researchers investigated the diet and health of a culture in Tukisenta, in the highlands of Papua New Guinea. The eat practically nothing but sweet potatoes, and their typical daily fare is 94.6 percent carbohydrate. Whether or not you believe that exact number, their diet was clearly extraordinarily high in carbohydrate. They administered 100g OGTTs and measured blood glucose at one hour, which is a very stringent OGTT. They compared the results to those obtained in the 1965 Tecumseh study (US) obtained by the same method. Here's what they found (
1):

Compared to Americans, in Tukisenta they had an extraordinary glucose tolerance at all ages. At one hour, their blood glucose was scarcely above normal fasting values, and glucose tolerance only decreased modestly with age. In contrast, in Americans over 50 years old, the
average one-hour value was around 180 mg/dL!
Now let's take a look at the African Bantu in the Lobaye region of the Central African Republic. The Bantu are a large ethnic group who primarily subsist on a diverse array of starchy foods including grains, beans, plantains and root crops. One hour after a 100g OGTT, their blood glucose was 113 mg/dL, compared to 139 mg/dL in American controls (
2). Those numbers are comparable to what investigators found in Tukisenta, and indicate an excellent glucose tolerance in the Bantu.
In South America, different investigators studied a group of native Americans in central Brazil that subsist primarily on cassava (a starchy root crop) and freshwater fish. Average blood glucose one hour after a 100g OGTT was 94 mg/dl, and only 2 out of 106 people tested had a reading over 160 mg/dL (both were older women) (
Western Diseases: Their Emergence and Prevention, p. 149). Again, that indicates a phenomenal glucose tolerance by Western standards.
I have to conclude that high-carbohydrate non-industrial cultures probably don't experience damaging high blood glucose levels, because their glucose tolerance is up to the task of shuttling a huge amount of glucose out of the bloodstream before that happens.
Not so fast...Now let's turn our attention to another study that may throw a wrench in the gears. A while back, I found a paper containing OGTT data for the !Kung San (also called the Bushmen), a hunter-gatherer group living in the Kalahari desert of Africa. I reported in an earlier post that they had a good glucose tolerance. When I revisited the paper recently, I realized I had misread it and in fact, their glucose tolerance was actually pretty poor.
Investigators administered a 50g OGTT, half what the other studies used. At one hour, the San had blood glucose readings of 169 mg/dL, compared to 142 mg/dL in Caucasian controls (
3)! I suspect a 100g OGTT would have put them close to the diabetic range.
Wait a minute, these guys are hunter-gatherers living the ancestral lifestyle; aren't they supposed to be super healthy?? First of all, like many hunter-gatherer groups the San are very small people: the men in this study were only 46 kg (101 lbs). The smaller you are, the more a given amount of carbohydrate will raise your blood glucose. Also, while I was mulling this over, I recalled a discussion where non-diabetic people were discussing their 'diabetic' OGTT values while on a low-carbohydrate diet. Apparently, carbohydrate refeeding for a few days generally reverses this and allows a normal OGTT in most people. It turns out this effect has been known for the better part of a century.
So what were the San eating? The study was conducted in October of 1970. The San diet changes seasonally, however their main staple food is the mongongo nut, which is mostly fat and which is available year-round (according to
The !Kung San: Men, Women and Work in a Foraging Society). Their carbohydrate intake is generally low by Western standards, and at times of the year it is very low. This varies by the availability of other foods, but they generally don't seem to relish the fibrous starchy root crops that are available in the area, as they mostly eat them when other food is scarce. Jean-Louis Tu has posted a nice analysis of the San diet on BeyondVeg (
4). Here's a photo of a San man collecting mongongo nuts from
The !Kung San: Men, Women and Work in a Foraging Society:

What did the authors of the OGTT study have to say about their diet? Acknowledging that prior carbohydrate intake may have played a role in the OGTT results of the San, they made the following remark:
a retrospective dietary history (M. J. Konner, personal communication, 1971) indicated that the [San], in fact, consumed fairly large amounts of carbohydrate-rich vegetable food during the week before testing.
However, the dietary history was not provided, nor has it been published, so we have no way to assess the statement's accuracy or what was meant by "fairly large amounts of carbohydrate-rich vegetable food." Given the fact that the San diet typically ranges from moderately low to very low in carbohydrate, I suspect they were not getting much carbohydrate as a percentage of calories. Looking at the nutritional value of the starchy root foods they typically eat in appendix D of
The !Kung San: Men, Women and Work in a Foraging Society, they are fibrous and most contain a low concentration of starch compared to a potato for example. The investigators may have been misled by the volume of these foods eaten, not realizing that they are not as rich in carbohydrate as the starchy root crops they are more familiar with.
You can draw your own conclusions, but I think the high OGTT result of the San probably reflect a low habitual carbohydrate intake, and not pre-diabetes. I have a very hard time believing that this culture wasn't able to handle the moderate amount of carbohydrate in their diet effectively, as observers have never described diabetic complications among them.
Putting it all togetherThis brings me to my hypothesis. I think a healthy human body is extraordinarily flexible in its ability to adapt to a very broad range of carbohydrate intakes, and adjusts glucose tolerance accordingly to maintain carbohydrate handling in a healthy range. In the context of a healthy diet and lifestyle (from birth), I suspect that nearly anyone can adjust to a very high carbohydrate intake without getting dangerous blood glucose spikes. A low carbohydrate intake leads to impaired glucose handling and better fat handling, as one would expect. This can show up as impaired glucose tolerance or even 'diabetes' on an OGTT, but that does not necessarily reflect a pathological state in my opinion.
Every person is different based on lifestyle, diet, personal history and genetics. Not everyone in affluent nations has a good glucose tolerance, and some people will never be able to handle starch effectively under any circumstances. The best way to know how your body reacts to carbohydrate is to test your own post-meal blood glucose using a glucose meter. They are inexpensive and work well. For the most informative result, eat a relatively consistent amount of carbohydrate for a week to allow your body to adapt, then take a glucose measurement 1 and 2 hours after a meal. If you don't eat much carbohydrate, eating a potato might make you think you're diabetic, whereas after a week of adaptation you may find that a large potato does not spike your blood glucose beyond the healthy range.
Exercise is a powerful tool for combating glucose intolerance, as it increases the muscles' demand for glucose, causing them to transport it out of the blood greedily after a meal. Any exercise that depletes muscle glycogen should be effective.
* Assuming a typical carbohydrate intake. Chris Kresser recently
argued, based on several studies, that true normal fasting glucose for a person eating a typical amount of carbohydrate is below 83 mg/dL. Low-carbohydrate eating may raise this number, but that doesn't necessarily indicate a pathological change. High-carbohydrate cultures such as the Kitavans, Aymara and New Guineans tend to have fasting values in the low 60s to low 70s. I suspect that a very high carbohydrate intake generally lowers fasting glucose in healthy people. That seems to be the case so far for Chris Voigt, on his diet of
20 potatoes a day. Stay tuned for an interview with Mr. Voigt in early December.