Adiponectin is a hormone exclusively secreted by body fat. This hormone has been recently gaining attention from researchers because of some of its functions. Two important ones are the regulation of glucose and fat metabolism.
Elevated levels of adiponectin are associated with increased insulin sensitivity, and increased fat catabolism (i.e., fat burning). And these associations appear to be causal. That is, adiponectin levels do not seem to be only markers, but causes of increased insulin sensitivity and fat catabolism.
In other words, an increase in circulating adiponectin seems to lead to increased insulin sensitivity and increased fat catabolism. Insulin sensitivity is the opposite of insulin resistance. The latter is a precursor to diabetes type 2, and is associated with elevated fasting and postprandial (i.e., after a meal) glucose levels.
Adiponectin also seems to work closely with leptin, another hormone implicated in a number of diseases of civilization. It appears that adiponecting and leptin modulate each other’s secretion and effects in metabolic processes.
So what do we do to increase our levels of circulating adiponectin?
Well, apparently there is only one guaranteed way, and that is to lose body fat!
Adiponectin is unique among hormones secreted by body fat in that it increases as body fat decreases. Other important body fat hormones, such as leptin, decrease with body fat loss.
The figure below (from: Poppitt et al., 2008) shows a graph where adiponectin levels are plotted against body mass index (BMI). BMI is strongly correlated with body fat percentage.
As you can see from the figure above adiponectin levels more than double when BMI goes from 26 to 20. One does not need to be obese to take advantage of this effect, and to benefit from having increased adiponectin levels.
The linear (Pearson) correlation between BMI and adiponectin levels is indicated as a high 0.551. The fluctuations around the line (the "line" looks more like a quasi-linear curve obtained through quadratic regression), which are why the correlation is not 1, are probably due chiefly to two factors:
- BMI is not a very precise measure of body fat. A very muscular person will have a high BMI and low body fat. That person will consequently have much higher adiponectin levels than an obese person with equal BMI.
- Adiponectin levels are naturally higher in women than in men. This is another point in favor of adiponectin, as women have always been the evolutionary bottleneck among our Paleolithic ancestors.
Now you know why doctors prescribe weight loss to patients with diabetes type 2.
And, when we look at various hunter-gatherer groups that were apparently free of diseases of civilization prior to westernization, there are only a few common denominators. Diet was not one of them, as Weston Price and others have shown us, at least not in the sense of what they included in their diet.
One of the few common denominators was arguably the fact that those hunter-gatherers typically had relatively low levels of body fat; an almost universal feature among non-westernized hunter-gatherers.
Reference:
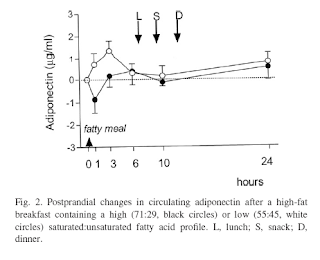
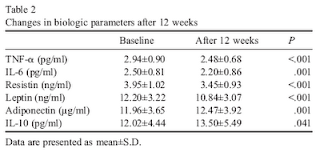
Poppitt, S.D. et al. (2008). Postprandial response of adiponectin, interleukin-6, tumor necrosis factor-α, and C-reactive protein to a high-fat dietary load. Nutrition, 24(4), 322-329.
Tuesday, March 30, 2010
Sunday, March 28, 2010
LDL, chylomicrons, HDL, and atherosclerosis: A lazy Sunday theory
Notes:
- This post is a joke, admittedly a weird one, which is why it is labeled “humor” and is filed under “Abstract humor”.
- I apologize for this spoiler. Some people probably like humor posts better if they do not know what they are in advance, but several others may think that reading a post like this is a waste of their time. If you are in the latter category, move on to another post! If not, here it goes …
Today I was spending some time under the sun, in one of the year’s 364 sunny days in Laredo, Texas. The goal was to see if I could obtain a precise count of the number of advanced glycation endproducts (a.k.a. AGEs) that would form as my skin was exposed to the sun’s damaging rays.
Then I read a post by Peter at Hyperlipid, and inspiration consumed me. A new theory was born regarding the interplay of LDL, chylomicrons, HDL, and atherosclerosis. By the way, Peter is a fat genius, by which I mean a genius regarding all fat issues – who happens to be thin.
A key observation forms the main pillar on which this new theory solidly rests:
The endothelium gaps, which let atherogenic particles enter into the forbidden area and do their damage, are around 25 nanometers in diameter. And what is the typical size of LDL particles? You guessed it, 25 nanometers in diameter! And guess what more, quite a few of the chylomicrons, another group of particles that would elicit immediate revulsion in any normal human being, are even smaller than 25 nanometers in diameter; those atherogenic pests!
So here is the theory, in a nutshell. A 500-page book will clearly be needed to discuss it in more detail.
The Devil created LDL particles to kill us all. But LDL particles were not such effective killers, because the Devil, trying to pack as much killer cholesterol into them, ended up making them too big! At 25 nanometers in diameter, on average, they basically had to squeeze their way into the forbidden area.
Since LDL particles were not doing a good enough job, the Devil also created chylomicrons, and those chaotic pests come in all sizes. In fact, it is well known that the word chylomicron has a Greek origin: chylo = killer, micron = particle (Deth & Disis, 1999; full reference at the end of this post).
And, needless to say, LDL particles and chylomicrons are fat particles that make the blood kind of taste and smell like butter, a toxic substance often fed to laboratory rats and known for its powerful carcinogenic properties among all living creatures except descendants of Vlad the Impaler. The latter has long been rumored to have been one of the Devil's best buddies, so no surprise there.
Michael the Archangel, who dislikes the Devil, and usually takes a hands-on approach to dealing with those he dislikes, the Devil in particular, gave us HDL particles. If you have any doubts about Michael’s hands-on approach, check the picture below (from: Wikipedia), which clearly shows what Michael had already done to the Devil. And that was over a relatively minor disagreement.
And don’t think about trying to discredit this theory by asking why HDL particles are so small compared with LDL particles and chylomicrons! This is easy. For the same reason that David was small and Goliath big!
But those nasty particles, the LDLs and chylomicrons, weren't only two big bullies, they were two against one. HDL particles were doing a valiant job at fighting the damage done by the Devil’s two evil particles, but not quite enough to save everybody from atherosclerosis.
Michael cried foul, and threatened to give the Devil another lesson. God, seeing this, said: Michael, no, mankind must be given a choice! If men and women want to gorge on the fatty flesh of the beasts they savagely slaughter, let them sin and face the consequences.
And so it was.
This theory probably needs some adjustments and refinements based on analysis of refereed research, especially solid research supported by drug manufacturers, and consultation with the most interesting man in the world. But I am pretty confident it can, after adjustments and refinements, pass the test of time.
The only nagging problem is the Original Sin. To the best of my knowledge, it was not eating the fatty flesh of beasts. It was eating a very sweet apple …
Reference:
Deth, R., & Disis, M. (1999, Feb 31). The origins of killer lipids: An evolutionary-theological perspective. The Lipid Review, 123(7), 77-66.
- This post is a joke, admittedly a weird one, which is why it is labeled “humor” and is filed under “Abstract humor”.
- I apologize for this spoiler. Some people probably like humor posts better if they do not know what they are in advance, but several others may think that reading a post like this is a waste of their time. If you are in the latter category, move on to another post! If not, here it goes …
***
Today I was spending some time under the sun, in one of the year’s 364 sunny days in Laredo, Texas. The goal was to see if I could obtain a precise count of the number of advanced glycation endproducts (a.k.a. AGEs) that would form as my skin was exposed to the sun’s damaging rays.
Then I read a post by Peter at Hyperlipid, and inspiration consumed me. A new theory was born regarding the interplay of LDL, chylomicrons, HDL, and atherosclerosis. By the way, Peter is a fat genius, by which I mean a genius regarding all fat issues – who happens to be thin.
A key observation forms the main pillar on which this new theory solidly rests:
The endothelium gaps, which let atherogenic particles enter into the forbidden area and do their damage, are around 25 nanometers in diameter. And what is the typical size of LDL particles? You guessed it, 25 nanometers in diameter! And guess what more, quite a few of the chylomicrons, another group of particles that would elicit immediate revulsion in any normal human being, are even smaller than 25 nanometers in diameter; those atherogenic pests!
So here is the theory, in a nutshell. A 500-page book will clearly be needed to discuss it in more detail.
The Devil created LDL particles to kill us all. But LDL particles were not such effective killers, because the Devil, trying to pack as much killer cholesterol into them, ended up making them too big! At 25 nanometers in diameter, on average, they basically had to squeeze their way into the forbidden area.
Since LDL particles were not doing a good enough job, the Devil also created chylomicrons, and those chaotic pests come in all sizes. In fact, it is well known that the word chylomicron has a Greek origin: chylo = killer, micron = particle (Deth & Disis, 1999; full reference at the end of this post).
And, needless to say, LDL particles and chylomicrons are fat particles that make the blood kind of taste and smell like butter, a toxic substance often fed to laboratory rats and known for its powerful carcinogenic properties among all living creatures except descendants of Vlad the Impaler. The latter has long been rumored to have been one of the Devil's best buddies, so no surprise there.
Michael the Archangel, who dislikes the Devil, and usually takes a hands-on approach to dealing with those he dislikes, the Devil in particular, gave us HDL particles. If you have any doubts about Michael’s hands-on approach, check the picture below (from: Wikipedia), which clearly shows what Michael had already done to the Devil. And that was over a relatively minor disagreement.
And don’t think about trying to discredit this theory by asking why HDL particles are so small compared with LDL particles and chylomicrons! This is easy. For the same reason that David was small and Goliath big!
But those nasty particles, the LDLs and chylomicrons, weren't only two big bullies, they were two against one. HDL particles were doing a valiant job at fighting the damage done by the Devil’s two evil particles, but not quite enough to save everybody from atherosclerosis.
Michael cried foul, and threatened to give the Devil another lesson. God, seeing this, said: Michael, no, mankind must be given a choice! If men and women want to gorge on the fatty flesh of the beasts they savagely slaughter, let them sin and face the consequences.
And so it was.
This theory probably needs some adjustments and refinements based on analysis of refereed research, especially solid research supported by drug manufacturers, and consultation with the most interesting man in the world. But I am pretty confident it can, after adjustments and refinements, pass the test of time.
The only nagging problem is the Original Sin. To the best of my knowledge, it was not eating the fatty flesh of beasts. It was eating a very sweet apple …
Reference:
Deth, R., & Disis, M. (1999, Feb 31). The origins of killer lipids: An evolutionary-theological perspective. The Lipid Review, 123(7), 77-66.
Labels:
cardiovascular disease,
cholesterol,
chylomicron,
HDL,
humor,
LDL
Friday, March 26, 2010
A trip to Europe: Some health-related routines and observations
Every year I travel to Europe on business, normally once or twice a year. These trips usually involve meetings with engineers, researchers, and project managers from various European countries; often 5 to 10 countries are represented.
Here are some of my notes on a recent trip to Europe. In this trip I spent time in two cities: Amsterdam, Netherlands and Antwerp, Belgium. Below is a set of the photos I took in Antwerp, of a statue depicting the roman soldier Silvius Brabo holding the severed hand of the giant Druon Antigoon.
According to legend Druon Antigoon had terrorized and extorted the people of Antwerp, cutting off the hands of several people and throwing them in the nearby Scheldt River, until the brave Silvius Brabo came into the scene and not only cut off the giant’s hand but also killed him.
This legend has probably been concocted toward the end of the Roman Empire, largely by the Romans, who first established Antwerp as a Roman outpost.
After this small digression, here are some health-related routines that I followed during this trip, and some of my main observations regarding diet and health issues.
On the plane:
- The meals were a festival of hyperglycemic and pro-inflammatory refined carbohydrates, unhealthy vegetable oils, and sugars – white bread, pasta, various sweets, pretzels, chips loaded with supposedly healthy omega 6 fats, margarine etc. I skipped all of the snacks and one of the meals, the breakfast. At the main meal of each flight I ate only meat, veggies, and some of the fruits.
- The flights over and back were very comfortable since I was water-fasting most of the time. Not a hint of indigestion or abdominal discomfort of any kind. These were 9 to 10 hour flights, from Houston to Amsterdam and back.
At business luncheons:
- The idea of having a sandwich for lunch seems to be getting popular in Europe. At least I have been seeing that happening more and more often lately. At these sandwich luncheons, I ate only the content of some sandwiches (basically cold cuts, cheese and veggies), and left the bread slices untouched.
- Some people noticed that I was not eating bread. I told them about insulin, lectins etc. A few looked at me as though I was insane; others with a disapproving look – dontchano, the lipid hypothesis!? A notable exception was a German gentleman who said that Germans were too pragmatic not to notice that they were getting fat on low fat diets, and are now reverting back to their staple diet of meats, fish, vegetable stews, and cheese.
At restaurants for dinner:
- This was fairly easy. I ate basically fish or meat dishes with veggies, and enjoyed them a lot. I skipped the deserts; again much to the surprise of some of my European colleagues.
- Skipping the desserts seems to have helped me cope with jetlag a lot better than I usually do. On my second day in Europe I slept quite well, and was unusually rested on the next day.
At the hotel:
- The breakfast buffets were a mix of: (a) breads, pastries, sweetened cereals, sugary items, and fruits; and (b) meats (often cured), some fish, cheeses, eggs, nuts, and some veggies. There were also fruit juices. I had solid breakfasts with (b)-type items, with a few fruits added (cantaloupe and berries). I had regular coffee with cream and no sugar, and stayed away from fruit juices.
- I did not use soap, shampoo etc. at the hotel; just plain water. Occasionally the soap used in hotels is very caustic, or rich in other chemicals, causing rashes. I stuck with showers and had no baths, as sometimes the bathtubs are not properly cleaned after their last use.
- At the end of my trip I took a train from Antwerp to Amsterdam, and stayed at a hotel near the Schiphol Airport (which has its own train station) since my flight back to the U.S. was in the morning. I had dinner by myself at the hotel, which was easy. I stopped at a place called Food Village at the Airport (visible from the Airport’s main entrance) and bought a water bottle, a piece of Gouda cheese, a can of sardines, and a box of seaweed. That was a very good dinner, and cost me about 6 euros.
The outcomes for me:
- I had no hint of indigestion at all throughout the trip, in spite of eating way more cheese than I normally do. The cheese that I ate was natural, aged cheese, not the processed kind.
- I had no need for more or less use of the bathroom than I usually do, and remained “regular” throughout the trip. No sign of constipation at all.
- I had no body odor (at least none that I could notice), even though I used no soap. My hair was fine too; I used no shampoo or conditioner.
- Jet lag problems were less pronounced than they usually are when I travel to Europe. The time difference is about 7 hours from Texas. Usually, I tend to feel very sleepy in the afternoon and wide awake around 3 am. Not this time.
- In spite of not exercising for about 7 days, except for walking, I was able to lift slightly heavier weights at a workout the day after my return than I did before my trip.
- According to the scale, I lost 1 pound during this trip. I do not know whether this was body fat or just water. It is unlikely that there was any muscle loss.
From what I could see, Europeans are generally thinner than Americans (particularly Texans), and also seem to be healthier. None of the people I met, not one, was clearly obese. On the other hand, the majority seemed to be somewhat overweight.
My impression was that the Europeans consume lesser amounts of refined carbohydrates and sugars than Americans, on a weekly basis, even though they currently consume more of those items than they should, in my opinion.
Consumption of vegetable oils other than olive oil is also lower than in the U.S; consumption of butter and cheese seems to be a lot higher.
From my conversations with several people during this trip, it seemed that the health of Europeans, like that of their American counterparts, is strongly correlated with the extent to which they are overweight. The more body fat, the more common was to hear complaints about pain here or there, fatigue, degenerative diseases, or talk about surgeries.
Here are some of my notes on a recent trip to Europe. In this trip I spent time in two cities: Amsterdam, Netherlands and Antwerp, Belgium. Below is a set of the photos I took in Antwerp, of a statue depicting the roman soldier Silvius Brabo holding the severed hand of the giant Druon Antigoon.
According to legend Druon Antigoon had terrorized and extorted the people of Antwerp, cutting off the hands of several people and throwing them in the nearby Scheldt River, until the brave Silvius Brabo came into the scene and not only cut off the giant’s hand but also killed him.
This legend has probably been concocted toward the end of the Roman Empire, largely by the Romans, who first established Antwerp as a Roman outpost.
After this small digression, here are some health-related routines that I followed during this trip, and some of my main observations regarding diet and health issues.
On the plane:
- The meals were a festival of hyperglycemic and pro-inflammatory refined carbohydrates, unhealthy vegetable oils, and sugars – white bread, pasta, various sweets, pretzels, chips loaded with supposedly healthy omega 6 fats, margarine etc. I skipped all of the snacks and one of the meals, the breakfast. At the main meal of each flight I ate only meat, veggies, and some of the fruits.
- The flights over and back were very comfortable since I was water-fasting most of the time. Not a hint of indigestion or abdominal discomfort of any kind. These were 9 to 10 hour flights, from Houston to Amsterdam and back.
At business luncheons:
- The idea of having a sandwich for lunch seems to be getting popular in Europe. At least I have been seeing that happening more and more often lately. At these sandwich luncheons, I ate only the content of some sandwiches (basically cold cuts, cheese and veggies), and left the bread slices untouched.
- Some people noticed that I was not eating bread. I told them about insulin, lectins etc. A few looked at me as though I was insane; others with a disapproving look – dontchano, the lipid hypothesis!? A notable exception was a German gentleman who said that Germans were too pragmatic not to notice that they were getting fat on low fat diets, and are now reverting back to their staple diet of meats, fish, vegetable stews, and cheese.
At restaurants for dinner:
- This was fairly easy. I ate basically fish or meat dishes with veggies, and enjoyed them a lot. I skipped the deserts; again much to the surprise of some of my European colleagues.
- Skipping the desserts seems to have helped me cope with jetlag a lot better than I usually do. On my second day in Europe I slept quite well, and was unusually rested on the next day.
At the hotel:
- The breakfast buffets were a mix of: (a) breads, pastries, sweetened cereals, sugary items, and fruits; and (b) meats (often cured), some fish, cheeses, eggs, nuts, and some veggies. There were also fruit juices. I had solid breakfasts with (b)-type items, with a few fruits added (cantaloupe and berries). I had regular coffee with cream and no sugar, and stayed away from fruit juices.
- I did not use soap, shampoo etc. at the hotel; just plain water. Occasionally the soap used in hotels is very caustic, or rich in other chemicals, causing rashes. I stuck with showers and had no baths, as sometimes the bathtubs are not properly cleaned after their last use.
- At the end of my trip I took a train from Antwerp to Amsterdam, and stayed at a hotel near the Schiphol Airport (which has its own train station) since my flight back to the U.S. was in the morning. I had dinner by myself at the hotel, which was easy. I stopped at a place called Food Village at the Airport (visible from the Airport’s main entrance) and bought a water bottle, a piece of Gouda cheese, a can of sardines, and a box of seaweed. That was a very good dinner, and cost me about 6 euros.
The outcomes for me:
- I had no hint of indigestion at all throughout the trip, in spite of eating way more cheese than I normally do. The cheese that I ate was natural, aged cheese, not the processed kind.
- I had no need for more or less use of the bathroom than I usually do, and remained “regular” throughout the trip. No sign of constipation at all.
- I had no body odor (at least none that I could notice), even though I used no soap. My hair was fine too; I used no shampoo or conditioner.
- Jet lag problems were less pronounced than they usually are when I travel to Europe. The time difference is about 7 hours from Texas. Usually, I tend to feel very sleepy in the afternoon and wide awake around 3 am. Not this time.
- In spite of not exercising for about 7 days, except for walking, I was able to lift slightly heavier weights at a workout the day after my return than I did before my trip.
- According to the scale, I lost 1 pound during this trip. I do not know whether this was body fat or just water. It is unlikely that there was any muscle loss.
From what I could see, Europeans are generally thinner than Americans (particularly Texans), and also seem to be healthier. None of the people I met, not one, was clearly obese. On the other hand, the majority seemed to be somewhat overweight.
My impression was that the Europeans consume lesser amounts of refined carbohydrates and sugars than Americans, on a weekly basis, even though they currently consume more of those items than they should, in my opinion.
Consumption of vegetable oils other than olive oil is also lower than in the U.S; consumption of butter and cheese seems to be a lot higher.
From my conversations with several people during this trip, it seemed that the health of Europeans, like that of their American counterparts, is strongly correlated with the extent to which they are overweight. The more body fat, the more common was to hear complaints about pain here or there, fatigue, degenerative diseases, or talk about surgeries.
Labels:
body fat,
cheese,
Europe,
my experience,
travel
Wednesday, March 24, 2010
More on the Harvard study on saturated versus polyunsaturated fats
This is a follow up on this post, which addressed the main argument put forth in a recent BBC article. The BBC article argued that people should replace saturated with polyunsaturated fats to reduce their risk of heart disease.
Let us take a look at the actual Harvard study itself (i.e., the study discussed in the BBC article). The Harvard study is linked here.
This post, by Stephan Guyenet, already pointed out several problems with the study. Stephan actually reviewed the studies used in the meta-analysis, and also some that were excluded in the meta-analysis and that he believes should have been included.
Here are a few other problems, in addition to the ones already pointed out by Stephan:
One thing that looks suspicious about this Harvard meta-analysis study is that they say that: “Statistical evidence for substantial between-study heterogeneity was not present (Q-statistic p = 0.13; I2 = 37%).”
A meta-analysis is a study that essentially summarizes, in a statistically sophisticated way, a bunch of other studies (the “sourced” studies). Too much between-study heterogeneity (i.e., widely disparate results among sourced studies) is undesirable, because it can bias the results.
The problem is similar to that of trying to summarize net worth figures (e.g., by calculating their average) in a middle class neighborhood that happens to have a few billionaires living in it. The heterogeneity in wealth may lead to a wildly overestimated average.
Now, we know that p values go down with sample size, and are usually high with small samples unless the effect measured by the statistic is very strong, regardless of the statistic used.
Well, with a sample of only 8 studies, their p value (associated with the Q statistic) is close to being significant at the 0.05 level!
If this sample of sourced studies were a little higher (say, 20), there would be significant between-study heterogeneity, which would call the meta-analysis into question. This is a big problem, since a good meta-analysis is expected to include a large number of studies (e.g., greater than 100), and this one included only 8 studies.
Moreover, to the best of my knowledge, the Q statistic is not very reliable when used with small samples, due to its low power as a test of heterogeneity. This makes the p value reported even more problematic.
Finally, the sourced study with the largest sample (n = 9,057; thus possibly the most credible), indicated as “Minnesota CS” on Figure 2 of the Harvard study, found increased risk of heart disease associated with increased consumption of polyunsaturated fats and reduced consumption of saturated fats.
Reference:
Mozaffarian, D., Micha, R., & Wallace, S. (2010). Effects on Coronary Heart Disease of Increasing Polyunsaturated Fat in Place of Saturated Fat: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS Med., 7(3): e1000252. doi: 10.1371/journal.pmed.1000252.
Let us take a look at the actual Harvard study itself (i.e., the study discussed in the BBC article). The Harvard study is linked here.
This post, by Stephan Guyenet, already pointed out several problems with the study. Stephan actually reviewed the studies used in the meta-analysis, and also some that were excluded in the meta-analysis and that he believes should have been included.
Here are a few other problems, in addition to the ones already pointed out by Stephan:
One thing that looks suspicious about this Harvard meta-analysis study is that they say that: “Statistical evidence for substantial between-study heterogeneity was not present (Q-statistic p = 0.13; I2 = 37%).”
A meta-analysis is a study that essentially summarizes, in a statistically sophisticated way, a bunch of other studies (the “sourced” studies). Too much between-study heterogeneity (i.e., widely disparate results among sourced studies) is undesirable, because it can bias the results.
The problem is similar to that of trying to summarize net worth figures (e.g., by calculating their average) in a middle class neighborhood that happens to have a few billionaires living in it. The heterogeneity in wealth may lead to a wildly overestimated average.
Now, we know that p values go down with sample size, and are usually high with small samples unless the effect measured by the statistic is very strong, regardless of the statistic used.
Well, with a sample of only 8 studies, their p value (associated with the Q statistic) is close to being significant at the 0.05 level!
If this sample of sourced studies were a little higher (say, 20), there would be significant between-study heterogeneity, which would call the meta-analysis into question. This is a big problem, since a good meta-analysis is expected to include a large number of studies (e.g., greater than 100), and this one included only 8 studies.
Moreover, to the best of my knowledge, the Q statistic is not very reliable when used with small samples, due to its low power as a test of heterogeneity. This makes the p value reported even more problematic.
Finally, the sourced study with the largest sample (n = 9,057; thus possibly the most credible), indicated as “Minnesota CS” on Figure 2 of the Harvard study, found increased risk of heart disease associated with increased consumption of polyunsaturated fats and reduced consumption of saturated fats.
Reference:
Mozaffarian, D., Micha, R., & Wallace, S. (2010). Effects on Coronary Heart Disease of Increasing Polyunsaturated Fat in Place of Saturated Fat: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS Med., 7(3): e1000252. doi: 10.1371/journal.pmed.1000252.
Tuesday, March 23, 2010
BBC article's advice: Replace saturated with polyunsaturated fats
The BBC article is here. It is based on meta-analysis of eight previous studies conducted by Harvard researchers, which the article states cover more than 13,000 people. The article also says that: “… [saturated] fats raise the levels of bad cholesterol that block the arteries to the heart.” They are of course referring to LDL cholesterol as the "bad cholesterol".
Sourcing bias is a notorious problem with meta-analyses (i.e., the choice of studies to use in a meta-analysis). Another problem is that you cannot tell what the studies sourced controlled for. Consider a study that compares health markers for smokers and non-smokers, where the smokers eat more saturated fat than the non-smokers. This study may confuse the effect of smoking with that of saturated fat consumption. To be reliable, the study must analyze the effect of saturated fat consumption, controlling for smoking habits.
There are other statistical issues to be considered in meta-analyses. For example, some of the sourced studies may take nonlinear relationships into consideration and others not. In multivariate analysis studies, nonlinearity may lead to significantly different results from those obtained through more conventional linear analyses.
Finally, reaching misleading results with sound statistical analyses is not that hard. As my age went from 1 to 20 years, my weight was strongly correlated with the price of gasoline. Yet, neither my weight caused the price of gasoline, nor the other way around. When you look at an individual study, not a meta-analysis, you can at least try to identify the possible sources of bias and mistakes.
Having said that, a solid refutation of the main argument in the article can be made from many angles. Here is a simple refutation based on what I would call the “HDL cholesterol angle”, with links to posts and various refereed publications:
- Increasing HDL cholesterol levels, especially beyond 60 mg/dl, dramatically decreases the risk of heart disease; and this is an almost universal effect in humans. This reduction in risk occurs even for people who suffer from diabetes and familial hypercholesterolemia. The latter is a genetic condition that is associated with very elevated LDL cholesterol and that is rare, typically afflicting 1 in 500 people in its heterozygous (and most common) form.
- Increasing consumption of saturated fats (present in: lard, fatty meat, coconut oil) and dietary cholesterol (from: fish, organ meats, eggs), while decreasing consumption of refined carbohydrates (e.g., pasta, white bread) and sugars (e.g., table sugar, high fructose corn syrup), significantly increases HDL cholesterol for the vast majority of people. Neither omega-6 nor omega-3 polyunsaturated fats lead to the same results. Omega-3 fats do reduce triglycerides, and increase HDL somewhat, but their effect on HDL pales in comparison with that of saturated fats. Excessive consumption of omega-6 fats is associated with chronic inflammation and related health problems.
- With the exception of cases involving familial hypercholesterolemia, there is no conclusive evidence that LDL cholesterol levels are associated with heart disease. Two widely used online calculators of risk of heart disease, based on the Framingham Heart Study and the Reynold Risk Score, do not even ask for LDL cholesterol levels to estimate risk. And that is not because they calculate LDL cholesterol based on other figures; they do not ask for VLDL cholesterol or triglycerides either.
After reading the BBC article again, it is clear that they are re-stating, in general terms, Rudolph Virchow’s mid-1800s lipid hypothesis. And they do so as if it was big news!
Sourcing bias is a notorious problem with meta-analyses (i.e., the choice of studies to use in a meta-analysis). Another problem is that you cannot tell what the studies sourced controlled for. Consider a study that compares health markers for smokers and non-smokers, where the smokers eat more saturated fat than the non-smokers. This study may confuse the effect of smoking with that of saturated fat consumption. To be reliable, the study must analyze the effect of saturated fat consumption, controlling for smoking habits.
There are other statistical issues to be considered in meta-analyses. For example, some of the sourced studies may take nonlinear relationships into consideration and others not. In multivariate analysis studies, nonlinearity may lead to significantly different results from those obtained through more conventional linear analyses.
Finally, reaching misleading results with sound statistical analyses is not that hard. As my age went from 1 to 20 years, my weight was strongly correlated with the price of gasoline. Yet, neither my weight caused the price of gasoline, nor the other way around. When you look at an individual study, not a meta-analysis, you can at least try to identify the possible sources of bias and mistakes.
Having said that, a solid refutation of the main argument in the article can be made from many angles. Here is a simple refutation based on what I would call the “HDL cholesterol angle”, with links to posts and various refereed publications:
- Increasing HDL cholesterol levels, especially beyond 60 mg/dl, dramatically decreases the risk of heart disease; and this is an almost universal effect in humans. This reduction in risk occurs even for people who suffer from diabetes and familial hypercholesterolemia. The latter is a genetic condition that is associated with very elevated LDL cholesterol and that is rare, typically afflicting 1 in 500 people in its heterozygous (and most common) form.
- Increasing consumption of saturated fats (present in: lard, fatty meat, coconut oil) and dietary cholesterol (from: fish, organ meats, eggs), while decreasing consumption of refined carbohydrates (e.g., pasta, white bread) and sugars (e.g., table sugar, high fructose corn syrup), significantly increases HDL cholesterol for the vast majority of people. Neither omega-6 nor omega-3 polyunsaturated fats lead to the same results. Omega-3 fats do reduce triglycerides, and increase HDL somewhat, but their effect on HDL pales in comparison with that of saturated fats. Excessive consumption of omega-6 fats is associated with chronic inflammation and related health problems.
- With the exception of cases involving familial hypercholesterolemia, there is no conclusive evidence that LDL cholesterol levels are associated with heart disease. Two widely used online calculators of risk of heart disease, based on the Framingham Heart Study and the Reynold Risk Score, do not even ask for LDL cholesterol levels to estimate risk. And that is not because they calculate LDL cholesterol based on other figures; they do not ask for VLDL cholesterol or triglycerides either.
After reading the BBC article again, it is clear that they are re-stating, in general terms, Rudolph Virchow’s mid-1800s lipid hypothesis. And they do so as if it was big news!
New Review of Controlled Trials Replacing Saturated fat with Industrial Seed Oils
Readers Stanley and JBG just informed me of a new review paper by Dr. Dariush Mozaffarian and colleagues. Dr. Mozaffarian is one of the Harvard epidemiologists responsible for the Nurse's Health study. The authors claim that overall, the controlled trials show that replacing saturated fat with polyunsaturated fat from industrial seed oils, but not carbohydrate or monounsaturated fat (as in olive oil), slightly reduces the risk of having a heart attack:
So basically, even if the authors' conclusion were correct, you overhaul your whole diet and replace natural foods with industrial foods, and...? You reduce your 10-year risk of having a heart attack from 10 percent to 9 percent. Without affecting your overall risk of dying. The paper states that the interventions didn't affect overall mortality.
* Not even single blinded. Autopsies were not conducted in a blinded manner. Physicians knew which hospital the cadavers came from, because autopsies were done on-site. There is some confusion about this point because the second paper states that physicians interpreted the autopsy reports in a blinded manner. But that doesn't make it blinded, since the autopsies weren't blinded. The patients were also not blinded, though this is hard to accomplish with a study like this.
** They refer to it as "cluster randomized", which I feel is a misuse of that term. The investigators definitely didn't randomize the individual patients: whichever hospital a person was being treated in, that's the food he/she ate. There were only two hospitals, so "cluster randomization" in this case would just refer to deciding which hospital got the intervention first. I don't think this counts as cluster randomization. An example of cluster randomization would be if you had 10 hospitals, and you randomized which hospital received which treatment first. It's analogous to individual randomization but on a group scale.
These findings provide evidence that consuming PUFA in place of SFA reduces CHD events in RCTs. This suggests that rather than trying to lower PUFA consumption, a shift toward greater population PUFA consumption in place of SFA would significantly reduce rates of CHD.Looking at the studies they included in their analysis (and at those they excluded), it looks like they did a nice job cherry picking. For example:
- They included the Finnish Mental Hospital trial, which is a terrible trial for a number of reasons. It wasn't randomized, properly controlled, or blinded*. Thus, it doesn't fit the authors' stated inclusion criteria, but they included it in their analysis anyway**. Besides, the magnitude of the result has never been replicated by better trials-- not even close.
- They included two trials that changed more than just the proportion of SFA to PUFA. For example, the Oslo Diet-heart trial replaced animal fat with seed oils, but also increased fruit, nut, vegetable and fish intake, while reducing trans fat margarine intake. The STARS trial increased both omega-6 and omega-3, reduced processed food intake, and increased fruit and vegetable intake. These obviously aren't controlled trials isolating the issue of dietary fat substitution. If you subtract the four inappropriate trials from their analysis, which is half the studies they analyzed, the significant result disappears. Those four just happened to show the largest reduction in heart attack mortality...
- They excluded the Rose et al. corn oil trial and the Sydney Diet-heart trial. Both found a large increase in total mortality from replacing animal fat with seed oils, and the Rose trial found a large increase in heart attack deaths (the Sydney trial reported total mortality but not CHD deaths).
So basically, even if the authors' conclusion were correct, you overhaul your whole diet and replace natural foods with industrial foods, and...? You reduce your 10-year risk of having a heart attack from 10 percent to 9 percent. Without affecting your overall risk of dying. The paper states that the interventions didn't affect overall mortality.
* Not even single blinded. Autopsies were not conducted in a blinded manner. Physicians knew which hospital the cadavers came from, because autopsies were done on-site. There is some confusion about this point because the second paper states that physicians interpreted the autopsy reports in a blinded manner. But that doesn't make it blinded, since the autopsies weren't blinded. The patients were also not blinded, though this is hard to accomplish with a study like this.
** They refer to it as "cluster randomized", which I feel is a misuse of that term. The investigators definitely didn't randomize the individual patients: whichever hospital a person was being treated in, that's the food he/she ate. There were only two hospitals, so "cluster randomization" in this case would just refer to deciding which hospital got the intervention first. I don't think this counts as cluster randomization. An example of cluster randomization would be if you had 10 hospitals, and you randomized which hospital received which treatment first. It's analogous to individual randomization but on a group scale.
Labels:
Cardiovascular disease,
diet,
disease,
fats
Monday, March 22, 2010
PepsiCo to reduce sugar and fat in products
I guess PepsiCo is moving ahead of the competition, but in a snail pace and in a very, very politically correct way. Will this help in any way? I doubt. It is just too little, too late. See article here.
The article states that:
The bottom line is that, if you want to improve your health, you should generally avoid any food or liquid that is highly industrialized.
Maybe PepsiCo should add unprocessed coconut water to their portfolio of drinks.
The article states that:
The company also set two goals for the next 10 years: to cut the average added sugar per serving by 25 percent and saturated fat per serving by 15 percent, in addition to adding more whole grains, fruits, vegetables and low-fat dairy into its array of products.While it is nice to see more of a focus on sugar than on saturated fat, I would have preferred to see something like this:
The company also set two goals for the next 5 years: to cut the average added sugar per serving by 95 percent and increase saturated fat per serving by 50 percent, in addition to adding more vegetables and full-fat dairy into its array of products.What would happen? Well, Indra Nooyi is a very smart CEO, and the company has many competent people. They know that they would probably lose enough customers to go out of business … or become the Apple of their industry.
The bottom line is that, if you want to improve your health, you should generally avoid any food or liquid that is highly industrialized.
Maybe PepsiCo should add unprocessed coconut water to their portfolio of drinks.
Labels:
coconut,
refined carbs,
saturated fat,
sugars
Saturday, March 20, 2010
Fatty Liver: It's not Just for Grown-ups Anymore
The epidemic of non-alcoholic fatty liver disease (NAFLD) is one of my favorite topics on this blog, due to the liver's role as the body's metabolic "grand central station", as Dr. Philip Wood puts it. The liver plays a critical part in the regulation of sugar, insulin, and lipid levels in the blood. Many of the routine blood tests administered in the doctor's office (blood glucose, cholesterol, etc.) partially reflect liver function.
NAFLD is an excessive accumulation of fat in the liver that impairs its function and can lead to severe liver inflammation (NASH), and in a small percentage of people, liver cancer. An estimated 20-30% of people in industrial nations suffer from NAFLD, a shockingly high prevalence (1).
I previously posted on dietary factors I believe are involved in NAFLD. In rodents, feeding a large amount of sugar or industrial seed oils (corn oil, etc.) promotes NAFLD, whereas fats such as butter and coconut oil do not (2). In human infants, enteric feeding with industrial seed oils causes severe liver damage, whereas the same amount of fat from fish oil doesn't, and can even reverse the damage done by seed oils (3). [2013 update: obesity is probably the main contributor to NAFLD. Obesity is associated with ectopic fat deposition in a number of organs, including the liver]
So basically, I think excessive sugar and industrial oils could be involved NAFLD, and if you look at diet trends in the US over the last 40 years, they're consistent with the idea.
I recently came across a study that examined the diet of Canadian children with NAFLD (6). The children had a high sugar intake, a typical (i.e., high) omega-6 intake, and a low omega-3 intake. The authors claimed that the children also had a high saturated fat intake, but at 10.5% of calories, they were almost eating to the American Heart Association's "Step I" diet recommendations**! Total fat intake was also low.
High sugar consumption was associated with a larger waist circumference, insulin resistance, lower adiponectin and elevated markers of inflammation. High omega-6 intake was associated with markers of inflammation. Low omega-3 intake was associated with insulin resistance and elevated liver enzymes. Saturated fat intake presumably had no relation to any of these markers, since they didn't mention it in the text.
These children with NAFLD, who were all insulin resistant and mostly obese, had diets high in omega-6, high in sugar, and low in omega-3. This is consistent with the idea that these three factors, which have all been moving in the wrong direction in the last 40 years, contribute to NAFLD.
* Fatty liver was assessed by liver enzymes, admittedly not a perfect test. However, elevated liver enzymes do correlate fairly well with NAFLD.
** Steps I and II were replaced by new diet advice in 2000. The AHA now recommends keeping saturated fat below 7% of calories. However, the new recommendations focus mostly on eating real food rather than avoiding saturated fat and cholesterol.
NAFLD is an excessive accumulation of fat in the liver that impairs its function and can lead to severe liver inflammation (NASH), and in a small percentage of people, liver cancer. An estimated 20-30% of people in industrial nations suffer from NAFLD, a shockingly high prevalence (1).
I previously posted on dietary factors I believe are involved in NAFLD. In rodents, feeding a large amount of sugar or industrial seed oils (corn oil, etc.) promotes NAFLD, whereas fats such as butter and coconut oil do not (2). In human infants, enteric feeding with industrial seed oils causes severe liver damage, whereas the same amount of fat from fish oil doesn't, and can even reverse the damage done by seed oils (3). [2013 update: obesity is probably the main contributor to NAFLD. Obesity is associated with ectopic fat deposition in a number of organs, including the liver]
So basically, I think excessive sugar and industrial oils could be involved NAFLD, and if you look at diet trends in the US over the last 40 years, they're consistent with the idea.
I recently came across a study that examined the diet of Canadian children with NAFLD (6). The children had a high sugar intake, a typical (i.e., high) omega-6 intake, and a low omega-3 intake. The authors claimed that the children also had a high saturated fat intake, but at 10.5% of calories, they were almost eating to the American Heart Association's "Step I" diet recommendations**! Total fat intake was also low.
High sugar consumption was associated with a larger waist circumference, insulin resistance, lower adiponectin and elevated markers of inflammation. High omega-6 intake was associated with markers of inflammation. Low omega-3 intake was associated with insulin resistance and elevated liver enzymes. Saturated fat intake presumably had no relation to any of these markers, since they didn't mention it in the text.
These children with NAFLD, who were all insulin resistant and mostly obese, had diets high in omega-6, high in sugar, and low in omega-3. This is consistent with the idea that these three factors, which have all been moving in the wrong direction in the last 40 years, contribute to NAFLD.
* Fatty liver was assessed by liver enzymes, admittedly not a perfect test. However, elevated liver enzymes do correlate fairly well with NAFLD.
** Steps I and II were replaced by new diet advice in 2000. The AHA now recommends keeping saturated fat below 7% of calories. However, the new recommendations focus mostly on eating real food rather than avoiding saturated fat and cholesterol.
Friday, March 19, 2010
Online calculators to assess cardiovascular disease risk: No LDL needed
Researchers can build mathematical equations (sometimes referred to as structural equations) that predict health outcomes based on health factors. Those mathematical equations can then be used in online calculators.
This link takes you to a government-sponsored calculator based on the Framingham Heart Study. It estimates 10-year risk for “hard” coronary heart disease outcomes (myocardial infarction and coronary death).
As you will notice, the link above does not take family history of disease into consideration. A different risk calculator, linked here, estimates a risk score called the Reynold Risk Score. It takes hsCRP (high sensitivity C-reactive protein, an inflammation marker) and family history in addition to the Framingham parameters in its risk score calculation.
Neither calculator asks for LDL cholesterol levels. I wonder why.
This link takes you to a government-sponsored calculator based on the Framingham Heart Study. It estimates 10-year risk for “hard” coronary heart disease outcomes (myocardial infarction and coronary death).
As you will notice, the link above does not take family history of disease into consideration. A different risk calculator, linked here, estimates a risk score called the Reynold Risk Score. It takes hsCRP (high sensitivity C-reactive protein, an inflammation marker) and family history in addition to the Framingham parameters in its risk score calculation.
Neither calculator asks for LDL cholesterol levels. I wonder why.
Labels:
cardiovascular disease,
cholesterol,
LDL,
research
Wednesday, March 17, 2010
Book Review: The Primal Blueprint
Mark Sisson has been a central figure in the evolutionary health community since he began his weblog Mark's Daily Apple in 2006. He and his staff have been posting daily on his blog ever since. He has also written several other books, edited the Optimum Health newsletter, competed as a high-level endurance athlete, and served on the International Triathlon Union as the anti-doping chairman, all of which you can read about on his biography page. Mark is a practice-what-you-preach kind of guy, and if physical appearance means anything, he's on to something.
In 2009, Mark published his long-awaited book The Primal Blueprint. He self-published the book, which has advantages and disadvantages. The big advantage is that you aren't subject to the sometimes onerous demands of publishers, who attempt to maximize sales at Barnes and Noble. The front cover sports a simple picture of Mark, rather than a sunbaked swimsuit model, and the back cover offers no ridiculous claims of instant beauty and fat loss.
The drawback of self-publishing is it's more difficult to break into a wider market. That's why Mark has asked me to publish my review of his book today. He's trying to push it up in the Amazon.com rankings so that it gets a broader exposure. If you've been thinking about buying Mark's book, now is a good time to do it. If you order it from Amazon.com on March 17th, Mark is offering to sweeten the deal with some freebies on his site Mark's Daily Apple. Full disclosure: I'm not getting anything out of this, I'm simply mentioning it because I was reviewing Mark's book anyway and I thought some readers might enjoy it.
The Primal Blueprint is not a weight loss or diet book, it's a lifestyle program with an evolutionary slant. Mark uses the example of historical and contemporary hunter-gatherers as a model, and attempts to apply those lessons to life in the 21st century. He does it in a way that's empowering accessible to nearly everyone. To illustrate his points, he uses the example of an archetypal hunter-gatherer called Grok, and his 21st century mirror image, the Korg family.
The diet section will be familiar to anyone who has read about "paleolithic"-type diets. He advocates eating meats including organs, seafood, eggs, nuts, abundant vegetables, and fruit. He also suggests avoiding grains, legumes, dairy (although he's not very militant about this one), processed food in general, and reducing carbohydrate to less than 150 grams per day. I like his diet suggestions because they focus on real food. Mark is not a drill sergeant. He tries to create a plan that will be sustainable in the long run, by staying positive and allowing for cheats.
We part ways on the issue of carbohydrate. He suggests that eating more than 150 grams of carbohydrate per day leads to fat gain and disease, whereas I feel that position is untenable in light of what we know of non-industrial cultures (including some relatively high-carbohydrate hunter-gatherers). Although carbohydrate restriction (or at least wheat and sugar restriction) does have its place in treating obesity and metabolic dysfunction in modern populations, ultimately I don't think it's necessary for the prevention of those same problems, and it can even be counterproductive in some cases. Mark does acknowledge that refined carbohydrates are the main culprits.
The book's diet section also recommends nutritional supplements, including a multivitamin/mineral, antioxidant supplement, probiotics, protein powder and fish oil. I'm not a big proponent of supplementation. I'm also a bit of a hypocrite because I do take small doses of fish oil (when I haven't had seafood recently), and vitamin D in wintertime. But I can't get behind protein powders and antioxidant supplements.
Mark's suggestions for exercise, sun exposure, sleep and stress management make good sense to me. In a nutshell: do all three, but keep the exercise varied and don't overdo it. As a former high-level endurance athlete, he has a lot of credibility here. He puts everything in a format that's practical, accessible and empowering.
I think The Primal Blueprint is a useful book for a person who wants to maintain or improve her health. Although we disagree on the issue of carbohydrate, the diet and lifestyle advice is solid and will definitely be a vast improvement over what the average person is doing. The Primal Blueprint is not an academic book, nor does it attempt to be. It doesn't contain many references (although it does contain some), and it won't satisfy someone looking for an in-depth discussion of the scientific literature. However, it's perfect for someone who's getting started and needs guidance, or who simply wants a more comprehensive source than reading blog snippets. It would make a great gift for that family member or friend who's been asking how you stay in such good shape.
In 2009, Mark published his long-awaited book The Primal Blueprint. He self-published the book, which has advantages and disadvantages. The big advantage is that you aren't subject to the sometimes onerous demands of publishers, who attempt to maximize sales at Barnes and Noble. The front cover sports a simple picture of Mark, rather than a sunbaked swimsuit model, and the back cover offers no ridiculous claims of instant beauty and fat loss.
The drawback of self-publishing is it's more difficult to break into a wider market. That's why Mark has asked me to publish my review of his book today. He's trying to push it up in the Amazon.com rankings so that it gets a broader exposure. If you've been thinking about buying Mark's book, now is a good time to do it. If you order it from Amazon.com on March 17th, Mark is offering to sweeten the deal with some freebies on his site Mark's Daily Apple. Full disclosure: I'm not getting anything out of this, I'm simply mentioning it because I was reviewing Mark's book anyway and I thought some readers might enjoy it.
The Primal Blueprint is not a weight loss or diet book, it's a lifestyle program with an evolutionary slant. Mark uses the example of historical and contemporary hunter-gatherers as a model, and attempts to apply those lessons to life in the 21st century. He does it in a way that's empowering accessible to nearly everyone. To illustrate his points, he uses the example of an archetypal hunter-gatherer called Grok, and his 21st century mirror image, the Korg family.
The diet section will be familiar to anyone who has read about "paleolithic"-type diets. He advocates eating meats including organs, seafood, eggs, nuts, abundant vegetables, and fruit. He also suggests avoiding grains, legumes, dairy (although he's not very militant about this one), processed food in general, and reducing carbohydrate to less than 150 grams per day. I like his diet suggestions because they focus on real food. Mark is not a drill sergeant. He tries to create a plan that will be sustainable in the long run, by staying positive and allowing for cheats.
We part ways on the issue of carbohydrate. He suggests that eating more than 150 grams of carbohydrate per day leads to fat gain and disease, whereas I feel that position is untenable in light of what we know of non-industrial cultures (including some relatively high-carbohydrate hunter-gatherers). Although carbohydrate restriction (or at least wheat and sugar restriction) does have its place in treating obesity and metabolic dysfunction in modern populations, ultimately I don't think it's necessary for the prevention of those same problems, and it can even be counterproductive in some cases. Mark does acknowledge that refined carbohydrates are the main culprits.
The book's diet section also recommends nutritional supplements, including a multivitamin/mineral, antioxidant supplement, probiotics, protein powder and fish oil. I'm not a big proponent of supplementation. I'm also a bit of a hypocrite because I do take small doses of fish oil (when I haven't had seafood recently), and vitamin D in wintertime. But I can't get behind protein powders and antioxidant supplements.
Mark's suggestions for exercise, sun exposure, sleep and stress management make good sense to me. In a nutshell: do all three, but keep the exercise varied and don't overdo it. As a former high-level endurance athlete, he has a lot of credibility here. He puts everything in a format that's practical, accessible and empowering.
I think The Primal Blueprint is a useful book for a person who wants to maintain or improve her health. Although we disagree on the issue of carbohydrate, the diet and lifestyle advice is solid and will definitely be a vast improvement over what the average person is doing. The Primal Blueprint is not an academic book, nor does it attempt to be. It doesn't contain many references (although it does contain some), and it won't satisfy someone looking for an in-depth discussion of the scientific literature. However, it's perfect for someone who's getting started and needs guidance, or who simply wants a more comprehensive source than reading blog snippets. It would make a great gift for that family member or friend who's been asking how you stay in such good shape.
Labels:
book review,
diet,
exercise,
low-carb,
paleolithic diet
Thursday, March 11, 2010
Ketosis, methylglyoxal, and accelerated aging: Fact or fiction?
Ketosis is a state typically associated with very low carbohydrate diets, such as the Atkins diet. In this state, the liver produces ketones based on fat (body fat or dietary fat). Unlike fats, ketones are water soluble and used by many tissues (including brain tissues) as a source of energy.
Unlike glucose and lipoprotein-bound fats (in VLDL, for example), unused ketones cannot be converted back to substances that can be stored by the body. Thus excess ketones are eliminated in the urine; leading to their detection by various tests, e.g., Ketostix tests.
This elimination of unused ketones in the urine is one of the reasons why very low carbohydrate diets are believed to lead to enhanced body fat loss.
From an evolutionary perspective, one could argue that a ketosis state that involves the elimination of ketones in the urine is an inefficient and unnatural emergency mechanism. For our Paleolithic ancestors, dying of starvation was a much bigger problem than dying of obesity complications.
An interesting hypothesis has been around for quite some time about a possible negative effect of ketosis. It goes more or less like this. Ketosis leads to the production of an organic compound called methylglyoxal, which is believed to be a powerful agent of glycation (a misnomer; see note below).
Glycation is a process whereby sugar molecules “stick” to protein or fat molecules, impairing their function. Glycation leads to the formation of advanced glycation endproducts (AGEs), which appear to be associated with a host of diseases, including diabetes, and to be implicated in accelerated aging (or “ageing”, with British spelling).
In short: ketosis leads to the production of methylglyoxal, which leads to the formation of AGEs, which in turn cause diseases and accelerated aging.
Note: Since glycation refers to “sugar” molecules sticking to protein and fats, its use in the context of methylglyoxal is arguably incorrect. Methylglyoxal is not a sugar, but an aldehyde.
One of the strongest indictments of ketosis, in relation to methylglyoxal, is made in a fairly well referenced book by De Grey (2007); the full reference to the book is at the end of this post. De Grey’s book is about aging, and how to stop or at least delay it. Overall, it is an excellent book. Here is some relevant text, from page 173 of the book:
Sorry, but I need to consult with my guru before I post my answer.
Reference:
De Grey, A. (2007). Ending aging: The rejuvenation breakthroughs that could reverse human aging in our lifetime. New York: NY: St. Martin’s Press.
Unlike glucose and lipoprotein-bound fats (in VLDL, for example), unused ketones cannot be converted back to substances that can be stored by the body. Thus excess ketones are eliminated in the urine; leading to their detection by various tests, e.g., Ketostix tests.
This elimination of unused ketones in the urine is one of the reasons why very low carbohydrate diets are believed to lead to enhanced body fat loss.
From an evolutionary perspective, one could argue that a ketosis state that involves the elimination of ketones in the urine is an inefficient and unnatural emergency mechanism. For our Paleolithic ancestors, dying of starvation was a much bigger problem than dying of obesity complications.
An interesting hypothesis has been around for quite some time about a possible negative effect of ketosis. It goes more or less like this. Ketosis leads to the production of an organic compound called methylglyoxal, which is believed to be a powerful agent of glycation (a misnomer; see note below).
Glycation is a process whereby sugar molecules “stick” to protein or fat molecules, impairing their function. Glycation leads to the formation of advanced glycation endproducts (AGEs), which appear to be associated with a host of diseases, including diabetes, and to be implicated in accelerated aging (or “ageing”, with British spelling).
In short: ketosis leads to the production of methylglyoxal, which leads to the formation of AGEs, which in turn cause diseases and accelerated aging.
Note: Since glycation refers to “sugar” molecules sticking to protein and fats, its use in the context of methylglyoxal is arguably incorrect. Methylglyoxal is not a sugar, but an aldehyde.
One of the strongest indictments of ketosis, in relation to methylglyoxal, is made in a fairly well referenced book by De Grey (2007); the full reference to the book is at the end of this post. De Grey’s book is about aging, and how to stop or at least delay it. Overall, it is an excellent book. Here is some relevant text, from page 173 of the book:
… one established effect of very low-carbohydrate diets of the Atkins type is to bring down both triglyceride levels and the body’s total exposure to carbohydrates, so some advocates have hypothesized that these diets world reduce a person’s AGE burden. Unfortunately, it turns out that the metabolic state that these diets induce (the notorious “ketosis”) has the unfortunate side effect of causing a jump in the production of the oxoaldehyde methylglyoxal, a major precursor of AGEs that is also, ironically, produced within cells of diabetic patients when they are forced to take in more glucose than they can immediately process … methylglyoxal is far more chemically reactive than blood sugar (up to 40,000 times more reactive, in fact), and is known to cause wide-ranging damage in the body, of which AGE cross-links are but one example. This potentially makes the Atkins diet a recipe for accelerated AGEing …Is this notion that ketosis, through methylglyoxal, can cause accelerated aging fact or fiction?
Sorry, but I need to consult with my guru before I post my answer.
Reference:
De Grey, A. (2007). Ending aging: The rejuvenation breakthroughs that could reverse human aging in our lifetime. New York: NY: St. Martin’s Press.
Vitamin D May Prevent Flu and Asthma
The AJCN just published a new controlled trial evaluating the effectiveness of vitamin D supplements on flu and asthma (1). Dr. Hiroyuki Ida's group gave Japanese schoolchildren (10 years average age) 1,200 IU of vitamin D3 or placebo per day from December through March. They found that children taking vitamin D had a significantly lower incidence of influenza A but not influenza B. These are two strains of flu that each accounted for roughly half the flu incidence in this population. Sadly, if you add the total flu incidence for A and B together (which the authors don't do in their tables), vitamin D supplementation didn't reduce total flu incidence significantly.
They also found that in the subset of children not already taking vitamin D supplements, the effect was greater, with unsupplemented children contracting nearly three times as many influenza A infections as children receiving vitamin D. They didn't analyze the influenza B or total influenza incidence in that way, so we don't know if prior supplementation makes a difference there.
The most striking finding of the paper is that the vitamin D group suffered from 6 times fewer asthma attacks than the placebo group. This needs to be repeated but it's consistent with other data and I find it very encouraging.
The paper did have some limitations. They didn't measure vitamin D status so they have no way to know exactly how effective their pill-based supplements were.
Another problem is that they began collecting data immediately after beginning supplementation. Vitamin D is a fat-soluble vitamin that can take 3 months to reach maximum concentration in the body following supplementation. By the time the children were reaching their maximum serum concentration of vitamin D, the trial was over. It would be nice to see the next trial begin supplementation in the fall and look at flu incidence in the winter.
This paper comes on the heels of another showing that vitamin D is necessary for the activation of an immune cell called the killer T cell (2). These are important for resistance to infections and cancer. Overall, these papers add to the accumulating evidence that vitamin D is important for the proper functioning of the human immune system. However, mice may not be the best model for use in studying vitamin D biology. From the first paper:
They also found that in the subset of children not already taking vitamin D supplements, the effect was greater, with unsupplemented children contracting nearly three times as many influenza A infections as children receiving vitamin D. They didn't analyze the influenza B or total influenza incidence in that way, so we don't know if prior supplementation makes a difference there.
The most striking finding of the paper is that the vitamin D group suffered from 6 times fewer asthma attacks than the placebo group. This needs to be repeated but it's consistent with other data and I find it very encouraging.
The paper did have some limitations. They didn't measure vitamin D status so they have no way to know exactly how effective their pill-based supplements were.
Another problem is that they began collecting data immediately after beginning supplementation. Vitamin D is a fat-soluble vitamin that can take 3 months to reach maximum concentration in the body following supplementation. By the time the children were reaching their maximum serum concentration of vitamin D, the trial was over. It would be nice to see the next trial begin supplementation in the fall and look at flu incidence in the winter.
This paper comes on the heels of another showing that vitamin D is necessary for the activation of an immune cell called the killer T cell (2). These are important for resistance to infections and cancer. Overall, these papers add to the accumulating evidence that vitamin D is important for the proper functioning of the human immune system. However, mice may not be the best model for use in studying vitamin D biology. From the first paper:
The evolution of different mechanisms for the regulation of PLC-γ1 activity in human and mouse T cells parallels the development of divergent VDR-dependent and VDR-independent antimicrobial pathways in human and mouse macrophages31, respectively, and may reflect the fact that mice are nocturnal animals with fur and humans are daytime creatures that synthesize vitamin D in the skin after exposure to ultraviolet light.In other words, mice don't use vitamin D in the same way as humans because they have a different evolutionary relationship to it.
Wednesday, March 10, 2010
A False Dichotomy
In the discussion section of the last post, the eternal argument about non-industrial people arose: were their lives (a) "nasty, brutish and short" (Hobbes), or were they (b) "noble savages" (Shaftesbury) living in Eden? The former argument states that they had awful lives, and we should be glad we're living int he 21st century. The latter argument implies that we should emulate them as much as possible. Each side is bursting with anecdotes to support their position.
Any time the discussion reaches this point, it stops providing us anything useful. The argument is a false dichotomy, one in which neither answer is correct. The correct answer is (c): none of the above. Some aspects of hunter-gatherer life are preferable to ours, and some aspects of our lives are preferable to theirs. Understanding that we spent a lot of evolutionary time as hunter-gatherers, as well as a few thousand years in small, tightly knit agricultural communities, may be useful in understanding how to work constructively with our own bodies and minds in the modern world.
So please, let's leave behind the false dichotomy and foster a more nuanced understanding of the lives our ancestors led.
Any time the discussion reaches this point, it stops providing us anything useful. The argument is a false dichotomy, one in which neither answer is correct. The correct answer is (c): none of the above. Some aspects of hunter-gatherer life are preferable to ours, and some aspects of our lives are preferable to theirs. Understanding that we spent a lot of evolutionary time as hunter-gatherers, as well as a few thousand years in small, tightly knit agricultural communities, may be useful in understanding how to work constructively with our own bodies and minds in the modern world.
So please, let's leave behind the false dichotomy and foster a more nuanced understanding of the lives our ancestors led.
Monday, March 8, 2010
The Paleolithic Mind
I went to a meditation retreat this week with the Red Cedar Zen community in Bellingham. It was a good experience. Staring at a wall from 6 am to 9 pm for a few days gives you the opportunity to learn a few things about your mind. Some of these are things you already know on some level, but you just need to have them reinforced. For example, the weight of psychological stress that we carry in modern societies like the US. It's only when it goes away for a while that you can see how heavy it was.
I'm totally ignorant of the scientific literature on this, but the way I see it, there are at least two main sources of psychological stress in the modern world for which we aren't well equipped as human beings:
The author says this about their possessions:
Unfortunately, we have more than just possessions on our minds. To live in the modern world is to be pricked to death by a thousand small responsibilities. Remember to make your lunch. Remember to make a doctor's appointment, shop for groceries, tie your shoes, get your oil changed, send that e-mail, make dinner, go for a jog, vacuum the floor, take a shower, pick up the kids-- the list is endless. Are our memories as defective as we think they are, or are we simply not designed to keep track of so many details?
In hunter-gatherer times, we had stress. Homicide, accidents, infectious disease and predation were always stalking us. But did we have a constant flow of obligations clogging the paths of our minds?
Those times are gone for us, but perhaps keeping them in mind can help us live more constructively in the modern world. I find that meditation helps keep the thousand pricks of modern life in perspective, perhaps bringing my mind closer to the paleolithic state.
I'm totally ignorant of the scientific literature on this, but the way I see it, there are at least two main sources of psychological stress in the modern world for which we aren't well equipped as human beings:
- Being eternally and inescapably subordinate in a large social structure
- Having too many responsibilities such as possessions and obligations
The Hadza do not engage in warfare [although they do have homicide]. They've never lived densely enough to be seriously threatened by an infectious outbreak. They have no known history of famine; rather, there is evidence of people from a farming group coming to live with them during a time of crop failure. The Hadza diet remains even today more stable and varied than that of most of the world's citizens. They enjoy an extraordinary amount of leisure time. Anthropologists have estimated that they "work"—actively pursue food—four to six hours a day. And over all these thousands of years, they've left hardly more than a footprint on the land.This isn't intended to idealize their lifestyle, but to point out that being a hunter-gatherer has its advantages. One of these is a minimal social structure in which each person is has full authority over himself:
The Hadza recognize no official leaders. Camps are traditionally named after a senior male (hence, Onwas's camp), but this honor does not confer any particular power. Individual autonomy is the hallmark of the Hadza. No Hadza adult has authority over any other. None has more wealth; or, rather, they all have no wealth. There are few social obligations—no birthdays, no religious holidays, no anniversaries.Even "marriage" doesn't carry much obligation. The author describes the Hadza as "serial monogamists". The idea of an eternal bond between two individuals doesn't exist. Women are not subordinate to men:
Gender roles are distinct, but for women there is none of the forced subservience knit into many other cultures. A significant number of Hadza women who marry out of the group soon return, unwilling to accept bullying treatment. Among the Hadza, women are frequently the ones who initiate a breakup—woe to the man who proves himself an incompetent hunter or treats his wife poorly. In Onwas's camp, some of the loudest, brashest members were women.Contrast this with modern civilizations in which everyone has a boss-- whether it's at a job, in a marriage or under your country's legal system. I think this feeling of perpetual subordination is destructive to an animal such as ourselves, that has spent so much of its existence mostly free of these pressures.
The author says this about their possessions:
Traditional Hadza, like Onwas and his camp mates, live almost entirely free of possessions. The things they own—a cooking pot, a water container, an ax—can be wrapped in a blanket and carried over a shoulder.This resembles other African hunter-gatherer groups that have few and simple tools. From the book The !Kung San: Men, Women and Work in a Foraging Society:
!Kung tools are few in number, lightweight, made from locally available materials, and multipurpose.Again, this is in sharp contrast to the modern world, where we have so many belongings it's impossible to keep track of them all. We have giant houses that we "need" to store all these things, and still it doesn't seem like enough. Many of our possessions are indispensable if we want to fit in to society. We need (or feel we need) clothes, cookware, identification, money, transportation, furniture, tools, sports gear, et cetera. Having to be responsible for this extraordinary quantity of possessions (by evolutionary standards) is a heavy weight on our minds.
Unfortunately, we have more than just possessions on our minds. To live in the modern world is to be pricked to death by a thousand small responsibilities. Remember to make your lunch. Remember to make a doctor's appointment, shop for groceries, tie your shoes, get your oil changed, send that e-mail, make dinner, go for a jog, vacuum the floor, take a shower, pick up the kids-- the list is endless. Are our memories as defective as we think they are, or are we simply not designed to keep track of so many details?
In hunter-gatherer times, we had stress. Homicide, accidents, infectious disease and predation were always stalking us. But did we have a constant flow of obligations clogging the paths of our minds?
Those times are gone for us, but perhaps keeping them in mind can help us live more constructively in the modern world. I find that meditation helps keep the thousand pricks of modern life in perspective, perhaps bringing my mind closer to the paleolithic state.
Labels:
Hadza,
meditation
Wednesday, March 3, 2010
Adiponectin and tumor necrosis factor-alpha levels after a high saturated fat meal
This is one of those interesting studies where the authors start with some pre-conceived assumptions and end up concluding something else, some way toward the opposite of what they assumed.
My final interpretation of the study results is a bit different though. It suggests that the results are actually the opposite of what the authors originally assumed.
The authors of the study (Poppitt et al., 2008; full reference at the end of this post) start by stating that since “… dietary fat is associated with increased lipid storage, weight gain, and obesity …” it is important to study the effect of dietary fat intake on the blood levels of certain substances that are associated with lipid disorders, weight gain and obesity.
In short, the authors start from the assumption that dietary fat is bad. By the way, this type of indictment of all fats is not very common these days. Usually saturated fat is the target.
Since dietary fat is assumed to be bad for us, that justifies the authors’ goal of studying the effect of dietary fat on certain hormones associated with bad health, including the body fat-secreted hormones adiponectin and tumor necrosis factor-alpha. Low levels of serum adiponectin, and elevated levels of tumor necrosis factor-alpha, are associated with various health complications.
In the study, a high-fat test meal with approximately 59 g of fat (71% of energy as fat) was given at breakfast on two occasions to 18 healthy and lean men. These men had, on average, 23 years of age, a 31-inch waist, and a body mass index of 22.9. In other words, they were young and fit.
Two fatty meal variations were used, one with a lot more saturated fat than the other. Their ratio of saturated:unsaturated fatty acids was 71:29 for the high saturated fat meal, and 55:45 for the other. The table below provides a more detailed picture of the fat composition of the meals. The authors refer to these meals as instances of “acute intake of dietary lipid”.
Lunch, snack and dinner meals were also served to the participants. Those meals were nearly fat-free, with 1 to 3 g of fat only; apparently to help the participants “recover” from the high fat meal. They included plenty of refined grains (e.g., pasta) and fruit juices. Way to go; give these folks refined carbohydrates and sugars galore to help them recover from the “damage” done by the high fat meal!
Blood samples were collected at 0 (baseline), 1, 3, and 6 h for the measurement of various substances, including the body fat hormones adiponectin and tumor necrosis factor-alpha levels.
The figure below shows the variation in adiponectin levels at several times after the meal. The black circles are for the high saturated fat group, and the white circles for the other group. Adiponectin levels do not really start at the same level for both groups, which makes the graph a bit unclear; to better interpret the graph it may be a good idea to simply ignore the first (white) circle at the zero mark on the vertical axis. Also, no hormone levels were negative, of course; the zero on the vertical axis represents a reference value.
As we can see from the figure above, adiponectin levels go up for both groups after the fatty meal, and end up higher than they started for both groups; more for the high saturated fat than for the low saturated fat group. They are at very similar levels at the 24 h mark, but the levels at 24 h for the high saturated fat group appear to be a lot higher than they were right after the fatty meal. (The start point for the high saturated fat group being the first black circle from the left on the graph.) None of the differences are reported as significant. This is not surprising, given the small sample.
The figure below shows the variation in tumor necrosis factor-alpha levels at several times after the meal. This is an even more interesting one, because it suggests a possible negative effect of the low fat meals.
In terms of tumor necrosis factor-alpha levels, the figure above suggests that both groups end up higher than they started, by about the same amount, which is not very good. (With tumor necrosis factor-alpha, unlike adiponectin, the less you have the better - so to speak, the hormone has important functions.) Again, none of the differences, with the exception of one, are reported as significant. The exception is the tumor necrosis factor-alpha level at 6 h for the low saturated fat group, which is significantly lower. But that difference disappears at the 10 h mark, never to be seen again.
Interestingly, note that tumor necrosis factor-alpha levels go up very clearly after the additional meals, which were low fat meals rich in refined carbohydrate and sugars. The variation in adiponectin is not as clearly associated with the additional meals. The points at which those meals were served are indicated by the arrows at the top of the graph; first arrow from left for lunch, second for a snack, and third arrow for dinner.
The conclusion by the authors of the study was that there is “… no evidence from this study of lean, healthy male subjects that the adipose hormone adiponectin is sensitive to acute intake of dietary lipid or to an increase in fatty acid saturation.” They do acknowledge the reduction in tumor necrosis factor-alpha up until the start of the low fat meals, and say that the “mechanism leading to the decrease in TNF-alpha on the high SFA:USFA treatment in our trial is unknown to us.”
My interpretation of this study is that, at least for young and lean men:
- There is some evidence that dietary saturated fat intake leads to increased levels of circulating adiponectin and decreased levels of tumor necrosis factor-alpha in the first few hours after a meal rich in saturated fat; with plenty of palmitic acid in it, by the way, of which animal fat is a great source. These are desirable and health-promoting hormonal responses.
- These is some evidence that meals high in refined carbohydrates and sugars increase levels of circulating tumor necrosis factor-alpha in the hours following the meals. Elevated levels of tumor necrosis factor-alpha are not good news; something that I guess is implied by the name of the hormone.
- There is some evidence that dietary saturated fat intake leads to an increase in adiponectin levels 24 h after a high fat meal, even when it is followed by low fat meals high in refined carbohydrates and sugars. This suggests a protective effect, which is in line with the hypothesis that adiponectin is not only a health marker by also a health-promoting hormone.
Due to the small sample used, none of the conclusions above is based on statistically significant results. More research is needed in the future, with larger samples. I am not sure it will happen though. This study’s findings were obviously accidental, and saturated fat phobia is still widespread.
Adiponectin is highly correlated with body weight, particularly weight associated with body fat mass. So, if you were able to achieve weight loss through a low carbohydrate diet involving a high consumption of saturated fat, there is absolutely no need to change that based on the results of this study.
Plus, saturated fat has the added benefit that it increases HDL cholesterol, the “good” cholesterol.
Reference:
Poppitt, S.D. et al. (2008). Postprandial response of adiponectin, interleukin-6, tumor necrosis factor-α, and C-reactive protein to a high-fat dietary load. Nutrition, 24(4), 322-329.
My final interpretation of the study results is a bit different though. It suggests that the results are actually the opposite of what the authors originally assumed.
The authors of the study (Poppitt et al., 2008; full reference at the end of this post) start by stating that since “… dietary fat is associated with increased lipid storage, weight gain, and obesity …” it is important to study the effect of dietary fat intake on the blood levels of certain substances that are associated with lipid disorders, weight gain and obesity.
In short, the authors start from the assumption that dietary fat is bad. By the way, this type of indictment of all fats is not very common these days. Usually saturated fat is the target.
Since dietary fat is assumed to be bad for us, that justifies the authors’ goal of studying the effect of dietary fat on certain hormones associated with bad health, including the body fat-secreted hormones adiponectin and tumor necrosis factor-alpha. Low levels of serum adiponectin, and elevated levels of tumor necrosis factor-alpha, are associated with various health complications.
In the study, a high-fat test meal with approximately 59 g of fat (71% of energy as fat) was given at breakfast on two occasions to 18 healthy and lean men. These men had, on average, 23 years of age, a 31-inch waist, and a body mass index of 22.9. In other words, they were young and fit.
Two fatty meal variations were used, one with a lot more saturated fat than the other. Their ratio of saturated:unsaturated fatty acids was 71:29 for the high saturated fat meal, and 55:45 for the other. The table below provides a more detailed picture of the fat composition of the meals. The authors refer to these meals as instances of “acute intake of dietary lipid”.
Lunch, snack and dinner meals were also served to the participants. Those meals were nearly fat-free, with 1 to 3 g of fat only; apparently to help the participants “recover” from the high fat meal. They included plenty of refined grains (e.g., pasta) and fruit juices. Way to go; give these folks refined carbohydrates and sugars galore to help them recover from the “damage” done by the high fat meal!
Blood samples were collected at 0 (baseline), 1, 3, and 6 h for the measurement of various substances, including the body fat hormones adiponectin and tumor necrosis factor-alpha levels.
The figure below shows the variation in adiponectin levels at several times after the meal. The black circles are for the high saturated fat group, and the white circles for the other group. Adiponectin levels do not really start at the same level for both groups, which makes the graph a bit unclear; to better interpret the graph it may be a good idea to simply ignore the first (white) circle at the zero mark on the vertical axis. Also, no hormone levels were negative, of course; the zero on the vertical axis represents a reference value.
As we can see from the figure above, adiponectin levels go up for both groups after the fatty meal, and end up higher than they started for both groups; more for the high saturated fat than for the low saturated fat group. They are at very similar levels at the 24 h mark, but the levels at 24 h for the high saturated fat group appear to be a lot higher than they were right after the fatty meal. (The start point for the high saturated fat group being the first black circle from the left on the graph.) None of the differences are reported as significant. This is not surprising, given the small sample.
The figure below shows the variation in tumor necrosis factor-alpha levels at several times after the meal. This is an even more interesting one, because it suggests a possible negative effect of the low fat meals.
In terms of tumor necrosis factor-alpha levels, the figure above suggests that both groups end up higher than they started, by about the same amount, which is not very good. (With tumor necrosis factor-alpha, unlike adiponectin, the less you have the better - so to speak, the hormone has important functions.) Again, none of the differences, with the exception of one, are reported as significant. The exception is the tumor necrosis factor-alpha level at 6 h for the low saturated fat group, which is significantly lower. But that difference disappears at the 10 h mark, never to be seen again.
Interestingly, note that tumor necrosis factor-alpha levels go up very clearly after the additional meals, which were low fat meals rich in refined carbohydrate and sugars. The variation in adiponectin is not as clearly associated with the additional meals. The points at which those meals were served are indicated by the arrows at the top of the graph; first arrow from left for lunch, second for a snack, and third arrow for dinner.
The conclusion by the authors of the study was that there is “… no evidence from this study of lean, healthy male subjects that the adipose hormone adiponectin is sensitive to acute intake of dietary lipid or to an increase in fatty acid saturation.” They do acknowledge the reduction in tumor necrosis factor-alpha up until the start of the low fat meals, and say that the “mechanism leading to the decrease in TNF-alpha on the high SFA:USFA treatment in our trial is unknown to us.”
My interpretation of this study is that, at least for young and lean men:
- There is some evidence that dietary saturated fat intake leads to increased levels of circulating adiponectin and decreased levels of tumor necrosis factor-alpha in the first few hours after a meal rich in saturated fat; with plenty of palmitic acid in it, by the way, of which animal fat is a great source. These are desirable and health-promoting hormonal responses.
- These is some evidence that meals high in refined carbohydrates and sugars increase levels of circulating tumor necrosis factor-alpha in the hours following the meals. Elevated levels of tumor necrosis factor-alpha are not good news; something that I guess is implied by the name of the hormone.
- There is some evidence that dietary saturated fat intake leads to an increase in adiponectin levels 24 h after a high fat meal, even when it is followed by low fat meals high in refined carbohydrates and sugars. This suggests a protective effect, which is in line with the hypothesis that adiponectin is not only a health marker by also a health-promoting hormone.
Due to the small sample used, none of the conclusions above is based on statistically significant results. More research is needed in the future, with larger samples. I am not sure it will happen though. This study’s findings were obviously accidental, and saturated fat phobia is still widespread.
Adiponectin is highly correlated with body weight, particularly weight associated with body fat mass. So, if you were able to achieve weight loss through a low carbohydrate diet involving a high consumption of saturated fat, there is absolutely no need to change that based on the results of this study.
Plus, saturated fat has the added benefit that it increases HDL cholesterol, the “good” cholesterol.
Reference:
Poppitt, S.D. et al. (2008). Postprandial response of adiponectin, interleukin-6, tumor necrosis factor-α, and C-reactive protein to a high-fat dietary load. Nutrition, 24(4), 322-329.
Monday, March 1, 2010
Book Review: S.P.E.E.D.
This book was sent to me by Matt Schoeneberger, who co-authored it with Jeff Thiboutot. Both have master's degrees in exercise science and health promotion. S.P.E.E.D. stands for Sleep, Psychology, Exercise, Environment and Diet. The authors have attempted to create a concise, comprehensive weight loss strategy based on what they feel is the most compelling scientific evidence available. It's subtitled "The Only Weight Loss Book Worth Reading". Despite the subtitle that's impossible to live up to, it was an interesting and well-researched book. It was a very fast read at 205 large-print pages including 32 pages of appendices and index.
I really appreciate the abundant in-text references the authors provided. I have a hard time taking a health and nutrition book seriously that doesn't provide any basis to evaluate its statements. There are already way too many people flapping their lips out there, without providing any outside support for their statements, for me to tolerate that sort of thing. Even well-referenced books can be a pain if the references aren't in the text itself. Schoeneberger and Thiboutot provided appropriate, accessible references for nearly every major statement in the book.
Chapter one, "What is a Healthy Weight", discusses the evidence for an association between body weight and health. They note that both underweight and obesity are associated with poor health outcomes, whereas moderate overweight isn't. While I agree, I continue to maintain that being fairly lean and appropriately muscled (which doesn't necessarily mean muscular) is probably optimal. The reason that people with a body mass index (BMI) considered to be "ideal" aren't healthier on average than people who are moderately overweight may have to do with the fact that many people with an "ideal" BMI are skinny-fat, i.e. have low muscle mass and too much abdominal fat.
Chapter 2, "Sleep", discusses the importance of sleep in weight regulation and overall health. They reference some good studies and I think they make a compelling case that it's important. Chapter 3, "Psychology", details psychological strategies to motivate and plan for effective weight loss.
Chapter 4, "Exercise", provides an exercise plan for weight loss. The main message: do it! I think they give a fair overview of the different categories of exercise and their relative merits, including high-intensity intermittent training (HIIT). However, the exercise regimen they suggest is intense and will probably lead to overtraining in many people. They recommend resistance training major, multi-joint exercises, 1-3 sets to muscular failure 2-4 days a week. I've been at the higher end of that recommendation and it made my joints hurt, plus I was weaker than when I strength trained less frequently. I think the lower end of their recommendation, 1 set of each exercise to failure twice a week, is more than sufficient to meet the goal of maximizing improvements in body composition in most people. My current routine is one brief strength training session and one sprint session per week (in addition to my leisurely cycle commute), which works well for me on a cost-benefit level. However, I was stronger when I was strength training twice a week and never going to muscular failure (a la Pavel Tsatsouline).
Chapter 5, "Environment", is an interesting discussion of different factors that promote excessive calorie intake, such as the setting of the meal, the company or lack thereof, and food presentation. While they support their statements very well with evidence from scientific studies, I do have a lingering doubt about these types of studies: as far as I know, they're all based on short-term interventions. Science would be a lot easier if short-term always translated to long term, but unfortunately that's not the case. For example, studies lasting one or two weeks show that low glycemic index foods cause a reduction in calorie intake and greater feelings of fullness. However, this effect disappears in the long term, and numerous controlled trials show that low glycemic index diets have no effect on food intake, body weight or insulin sensitivity in the long term. I reviewed those studies here.
The body has homeostatic mechanisms (homeostatic = maintains the status quo) that regulate long-term energy balance. Whether short-term changes in calorie intake based on environmental cues would translate into sustained changes that would have a significant impact on body fat, I don't know. For example, if you eat a meal with your extended family at a restaurant that serves massive portions, you might eat twice as much as you would by yourself in your own home. But the question is, will your body factor that huge meal into your subsequent calorie intake and energy expenditure over the following days? The answer is clearly yes, but the degree of compensation is unclear. Since I'm not aware of any trials indicating that changing meal context can actually lead to long-term weight loss, I can't put much faith in this strategy (if you know otherwise, please link to the study in the comments).
Chapter 6, "Diet", is a very brief discussion of what to eat for weight loss. They basically recommend a low-calorie, low-carb diet focused on whole, natural foods. I think low-carbohydrate diets can be useful for some overweight people trying to lose weight, if for no other reason than the fact that they make it easier to control appetite. In addition, a subset of people respond very well to carbohydrate restriction in terms of body composition, health and well-being. The authors emphasize nutrient density, but don't really explain how to achieve it. It would have been nice to see a discussion of a few topics such as organ meats, leafy greens, dairy quality (pastured vs. conventional) and vitamin D. These may not help you lose weight, but they will help keep you healthy, particularly on a calorie-restricted diet. The authors also recommend a few energy bars, powders and supplements that I don't support. They state that they have no financial connection to the manufacturers of the products they recommend.
I'm wary of their recommendation to deliberately restrict calorie intake. Although it will clearly cause fat loss if you restrict calories enough, it's been shown to be ineffective for sustainable, long-term fat loss over and over again. The only exception is the rare person with an iron will who is able to withstand misery indefinitely. I'm going to keep an open mind on this question though. There may be a place for deliberate calorie restriction in the right context. But at this point I'm going to require some pretty solid evidence that it's effective, sustainable, and doesn't have unacceptable side effects.
The book contains a nice bonus, an appendix titled "What is Quality Evidence"? It's a brief discussion of common logical pitfalls when evaluating evidence, and I think many people could benefit from reading it.
Overall, S.P.E.E.D. was a worthwhile read, definitely superior to 95% of fat loss books. With some caveats mentioned above, I think it could be a useful resource for someone interested in fat loss.
I really appreciate the abundant in-text references the authors provided. I have a hard time taking a health and nutrition book seriously that doesn't provide any basis to evaluate its statements. There are already way too many people flapping their lips out there, without providing any outside support for their statements, for me to tolerate that sort of thing. Even well-referenced books can be a pain if the references aren't in the text itself. Schoeneberger and Thiboutot provided appropriate, accessible references for nearly every major statement in the book.
Chapter one, "What is a Healthy Weight", discusses the evidence for an association between body weight and health. They note that both underweight and obesity are associated with poor health outcomes, whereas moderate overweight isn't. While I agree, I continue to maintain that being fairly lean and appropriately muscled (which doesn't necessarily mean muscular) is probably optimal. The reason that people with a body mass index (BMI) considered to be "ideal" aren't healthier on average than people who are moderately overweight may have to do with the fact that many people with an "ideal" BMI are skinny-fat, i.e. have low muscle mass and too much abdominal fat.
Chapter 2, "Sleep", discusses the importance of sleep in weight regulation and overall health. They reference some good studies and I think they make a compelling case that it's important. Chapter 3, "Psychology", details psychological strategies to motivate and plan for effective weight loss.
Chapter 4, "Exercise", provides an exercise plan for weight loss. The main message: do it! I think they give a fair overview of the different categories of exercise and their relative merits, including high-intensity intermittent training (HIIT). However, the exercise regimen they suggest is intense and will probably lead to overtraining in many people. They recommend resistance training major, multi-joint exercises, 1-3 sets to muscular failure 2-4 days a week. I've been at the higher end of that recommendation and it made my joints hurt, plus I was weaker than when I strength trained less frequently. I think the lower end of their recommendation, 1 set of each exercise to failure twice a week, is more than sufficient to meet the goal of maximizing improvements in body composition in most people. My current routine is one brief strength training session and one sprint session per week (in addition to my leisurely cycle commute), which works well for me on a cost-benefit level. However, I was stronger when I was strength training twice a week and never going to muscular failure (a la Pavel Tsatsouline).
Chapter 5, "Environment", is an interesting discussion of different factors that promote excessive calorie intake, such as the setting of the meal, the company or lack thereof, and food presentation. While they support their statements very well with evidence from scientific studies, I do have a lingering doubt about these types of studies: as far as I know, they're all based on short-term interventions. Science would be a lot easier if short-term always translated to long term, but unfortunately that's not the case. For example, studies lasting one or two weeks show that low glycemic index foods cause a reduction in calorie intake and greater feelings of fullness. However, this effect disappears in the long term, and numerous controlled trials show that low glycemic index diets have no effect on food intake, body weight or insulin sensitivity in the long term. I reviewed those studies here.
The body has homeostatic mechanisms (homeostatic = maintains the status quo) that regulate long-term energy balance. Whether short-term changes in calorie intake based on environmental cues would translate into sustained changes that would have a significant impact on body fat, I don't know. For example, if you eat a meal with your extended family at a restaurant that serves massive portions, you might eat twice as much as you would by yourself in your own home. But the question is, will your body factor that huge meal into your subsequent calorie intake and energy expenditure over the following days? The answer is clearly yes, but the degree of compensation is unclear. Since I'm not aware of any trials indicating that changing meal context can actually lead to long-term weight loss, I can't put much faith in this strategy (if you know otherwise, please link to the study in the comments).
Chapter 6, "Diet", is a very brief discussion of what to eat for weight loss. They basically recommend a low-calorie, low-carb diet focused on whole, natural foods. I think low-carbohydrate diets can be useful for some overweight people trying to lose weight, if for no other reason than the fact that they make it easier to control appetite. In addition, a subset of people respond very well to carbohydrate restriction in terms of body composition, health and well-being. The authors emphasize nutrient density, but don't really explain how to achieve it. It would have been nice to see a discussion of a few topics such as organ meats, leafy greens, dairy quality (pastured vs. conventional) and vitamin D. These may not help you lose weight, but they will help keep you healthy, particularly on a calorie-restricted diet. The authors also recommend a few energy bars, powders and supplements that I don't support. They state that they have no financial connection to the manufacturers of the products they recommend.
I'm wary of their recommendation to deliberately restrict calorie intake. Although it will clearly cause fat loss if you restrict calories enough, it's been shown to be ineffective for sustainable, long-term fat loss over and over again. The only exception is the rare person with an iron will who is able to withstand misery indefinitely. I'm going to keep an open mind on this question though. There may be a place for deliberate calorie restriction in the right context. But at this point I'm going to require some pretty solid evidence that it's effective, sustainable, and doesn't have unacceptable side effects.
The book contains a nice bonus, an appendix titled "What is Quality Evidence"? It's a brief discussion of common logical pitfalls when evaluating evidence, and I think many people could benefit from reading it.
Overall, S.P.E.E.D. was a worthwhile read, definitely superior to 95% of fat loss books. With some caveats mentioned above, I think it could be a useful resource for someone interested in fat loss.
Labels:
exercise,
overweight
Adiponectin, inflammation, diabetes, and heart disease
Humans, like many animals, evolved to be episodic eaters and spend most of their time fasting. Body fat is the main store of energy in the human body. Excess dietary carbohydrates and fat are stored as body fat, in specialized cells known as adipocytes. Excess dietary protein is not normally stored as body fat.
Adipocytes can be seen as being part of a very important and distributed endocrine organ, being responsible for the release of many different hormones into the bloodstream. One of these hormones is adiponectin. Other important hormones secreted by body fat tissue are leptin and tumor necrosis factor-alpha.
Among hormones, adiponectin is particularly interesting because it is negatively correlated with body fat mass. That is, unlike other hormones such as leptin and tumor necrosis factor-alpha, a decrease in body fat mass (a well known health marker) is associated with an increase in adiponectin. This has led some researchers to speculate that adiponectin is a causative factor that promotes health, in addition to being a health marker.
Jung and colleagues (2008; full reference at the end of this post) studied 78 obese individuals (41 females) who participated in an exercise program during 12 weeks. The exercise program involved mostly low intensity aerobic activities, such as brisk walking. The individuals also took an appetite suppressant, with the goal of reducing their calorie intake by about 500 kcal per day.
The table below (click on it to enlarge) shows various measurements for the participants before and after the 12-week intervention.
Adipocytes can be seen as being part of a very important and distributed endocrine organ, being responsible for the release of many different hormones into the bloodstream. One of these hormones is adiponectin. Other important hormones secreted by body fat tissue are leptin and tumor necrosis factor-alpha.
Among hormones, adiponectin is particularly interesting because it is negatively correlated with body fat mass. That is, unlike other hormones such as leptin and tumor necrosis factor-alpha, a decrease in body fat mass (a well known health marker) is associated with an increase in adiponectin. This has led some researchers to speculate that adiponectin is a causative factor that promotes health, in addition to being a health marker.
Jung and colleagues (2008; full reference at the end of this post) studied 78 obese individuals (41 females) who participated in an exercise program during 12 weeks. The exercise program involved mostly low intensity aerobic activities, such as brisk walking. The individuals also took an appetite suppressant, with the goal of reducing their calorie intake by about 500 kcal per day.
The table below (click on it to enlarge) shows various measurements for the participants before and after the 12-week intervention.
From the table above we can say that there were significant reductions in weight, body mass index (BMI), waist and hip circumference, waist-to-hip ratio (WHR), total body fat, and total fasting cholesterol and triglycerides. However, the participants were still obese at the end of the intervention, with an average body fat percentage of 35.5.
The table below shows the concentrations of various hormones secreted by body fat tissue, as well as other types of tissue, before and after the 12-week intervention. These hormones are all believed to be health indicators and/or health causes.
The table below shows the concentrations of various hormones secreted by body fat tissue, as well as other types of tissue, before and after the 12-week intervention. These hormones are all believed to be health indicators and/or health causes.
We see from the table above that the hormonal changes were all significant (all at the P < .001 level except one, at the P < .05 level), and all indicative of health improvements. The serum concentrations of all hormones decreased, with two exceptions – adiponectin and interleukin-10, which increased. Interleukin-10 is an anti-inflammatory hormone produced by white blood cells. The most significant increase of the two was by far in adiponectin (P = .001, versus P = .041 for interleukin-10).
One of the most promising effects of adiponectin seems to be an increase in insulin sensitivity. This effect appears to be unrelated to any effects on insulin secretion. That is, adiponectin seems to act directly on various cells, including muscle cells, increasing their ability to clear glucose from the blood. This effect seems to be one of the underlying, and previously unknown, reasons why loss of body fat improves health in those who suffer from diabetes type 2.
Increased serum adiponectin has been found to be significantly associated with: decreased body fat and particularly visceral fat, decreased risk of developing diabetes type 2, decreased blood pressure, and decreased fasting triglycerides.
Adiponectin appears to also have anti-inflammatory and athero-protective properties.
On average, women have higher levels of serum adiponectin than men.
According to Giannessi and colleagues (2007) administration of adiponectin in mice has shown positive results. Since research on adiponectin is new, it will probably be some time until related drugs are developed. Giannessi and colleagues also note that fish oil and vanadium salts may increase the synthesis and release of adiponectin.
So far it seems that the most effective way of increasing adiponectin levels is weight loss, particularly through body fat loss. Even as new drugs are developed, this will likely remain the most natural and safe way of increasing adiponectin levels.
All of this helps in the identification of missing links between body fat loss and health improvement. It seems that losing body fat has an effect similar to that of supplementation; it increases the blood concentration of a health-promoting substance - adiponectin!
References:
Giannessi, D., Maltinti, M., & Del Ry, S. (2007). Adiponectin circulating levels: A new emerging biomarker of cardiovascular risk. Pharmacological Research, 56(6), 459-467.
Gil-Campos, M., Cañete, R., & Gil, A. (2004). Adiponectin, the missing link in insulin resistance and obesity. Clinical Nutrition, 23(5), 963-974.
Jung, S.H. et al. (2008). Effect of weight loss on some serum cytokines in human obesity: increase in IL-10 after weight loss. The Journal of Nutritional Biochemistry, 19(6), 371-375.
One of the most promising effects of adiponectin seems to be an increase in insulin sensitivity. This effect appears to be unrelated to any effects on insulin secretion. That is, adiponectin seems to act directly on various cells, including muscle cells, increasing their ability to clear glucose from the blood. This effect seems to be one of the underlying, and previously unknown, reasons why loss of body fat improves health in those who suffer from diabetes type 2.
Increased serum adiponectin has been found to be significantly associated with: decreased body fat and particularly visceral fat, decreased risk of developing diabetes type 2, decreased blood pressure, and decreased fasting triglycerides.
Adiponectin appears to also have anti-inflammatory and athero-protective properties.
On average, women have higher levels of serum adiponectin than men.
According to Giannessi and colleagues (2007) administration of adiponectin in mice has shown positive results. Since research on adiponectin is new, it will probably be some time until related drugs are developed. Giannessi and colleagues also note that fish oil and vanadium salts may increase the synthesis and release of adiponectin.
So far it seems that the most effective way of increasing adiponectin levels is weight loss, particularly through body fat loss. Even as new drugs are developed, this will likely remain the most natural and safe way of increasing adiponectin levels.
All of this helps in the identification of missing links between body fat loss and health improvement. It seems that losing body fat has an effect similar to that of supplementation; it increases the blood concentration of a health-promoting substance - adiponectin!
References:
Giannessi, D., Maltinti, M., & Del Ry, S. (2007). Adiponectin circulating levels: A new emerging biomarker of cardiovascular risk. Pharmacological Research, 56(6), 459-467.
Gil-Campos, M., Cañete, R., & Gil, A. (2004). Adiponectin, the missing link in insulin resistance and obesity. Clinical Nutrition, 23(5), 963-974.
Jung, S.H. et al. (2008). Effect of weight loss on some serum cytokines in human obesity: increase in IL-10 after weight loss. The Journal of Nutritional Biochemistry, 19(6), 371-375.
Subscribe to:
Posts (Atom)